Journal of Vaccines & Immunization
An International Peer-Reviewed Open Access Journal
ISSN 2053-1273

- Download PDF
- |
- Download Citation
- |
- Email a Colleague
- |
- Share:
-
- Tweet
-

Journal of Vaccines & Immunization
Volume 3, Issue 1, February 2015, Pages 1–6
Short reportOpen Access
Impact of strategies and activities for reducing morbidity and mortality of vaccine-preventable diseases in Oman: A status report
- 1 Office of Undersecretary of Health Affairs, Ministry of Health, Muscat, Oman
*Corresponding author:Salah Thabit Al Awaidy, Communicable Disease Advisor to Health Affairs, Office of HE Undersecretary of Health Affairs, Ministry of Health, Muscat, Post Box 393 Postal Code 113, Sultanate of Oman. Tel.: +968 24946382 (O); Fax: +968 2494638; E-mail: salah.awaidy@gmail.com
Received 11 November 2014 Revised 12 January 2014 Accepted 22 January 2014 Published 30 January 2014
DOI: http://dx.doi.org/10.14312/2053-1273.2015-1
Copyright: © 2015 Al Awaidy ST. et al. Published by NobleResearch Publishers. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
AbstractTop
Immunization is the only child survival strategy which alone averts two to three million deaths each year. This has been possible because of high coverages achieved by many countries in the world. Still nearly 1.5 million children die of vaccine preventable diseases each year, mainly because of poor uptake of vaccines particularly in developing and under-developed countries. This calls for a detailed review and study of the successful models in countries which have consistently achieved high immunization coverage. Oman is one of those countries which has maintained more than 95% immunization coverage for more than a decade. The outcome has been that in Oman the incidence of vaccine preventable diseases has continued to remain low. The three major pillars behind the success of the immunization programme in Oman have been national expended programme of immunization, surveillance network and efficient supply chain system.
Keywords: vaccine preventable diseases; extended programme of immunization; Oman; immunization coverage; VPD surveillance; EPI target diseases
IntroductionTop
Despite of many countries being successful in achieving a high coverage the overall global picture is still grim especially for newer vaccines. Global coverage with three doses of Hib vaccine is estimated at 52%, for three doses of hepatitis B vaccine is estimated at 81%, for rotavirus, coverage was estimated at 14%. Thus in 2012, an estimated 21.8 million infants worldwide had not been covered by routine immunization services [1].
In May 2012, the World Health Assembly introduced the Global Vaccine Action Plan (GVAP) which was endorsed by 194 Member states [2]. The mission of this initiative is to improve health by extending the full benefits of immunization to all people till 2020 and beyond, regardless of where they are born, who they are or where they live. This is to be achieved using existing partnerships and coordinating mechanisms to support adapting the GVAP to the regional and country level. One of the goals of GVAP is to “meet vaccination coverage targets in every region, country and community” [2]. Thus, while there is focus on achieving the targets of immunization coverage in countries where it is low, the countries with high immunization coverage have to focus on maintaining it. The means by which high immunization coverage was achieved in these countries may serve as a model to achieve similar success in poor performing countries.
The focus of this paper is to monitor and assess the impact of strategies and activities for reducing morbidity and mortality of vaccine preventable diseases in Oman.
Status of vaccine preventable diseasesTop
The Expanded Program on Immunization (EPI) in Oman was launched in 1981. Since then, numerous efforts have been made to ensure the expansion of EPI at the grass roots level [3]. EPI has been integrated into the Primary Health Care (PHC) services provided by the Ministry of Health. The immunization coverage levels have increased substantially from 10% in 1981 to over 95% in 1995 [3]. The near 100% coverage among eligible persons has been maintained nationally and at provincials resulting in a significant impact on the incidence of vaccine preventable diseases in Oman. The administrative coverage has been confirmed by periodic validation of the vaccination coverage data using data quality self-assessment (DQS) every 3 years and coverage evaluation surveys every 5 years, the last one which was conducted in 2008 and the results were consistent with the administrative coverages in the country [4].
This has been possible due to the successful strategic models which ensure high coverage levels, such as the strong political commitment to the EPI within Ministry of Health (MoH), the implementation of the EPI policies which are carried out by the EPI static units located within the health institutions, single administrative control for EPI and cold chain management, integration of EPI services into the ‘Primary Health Care’, decentralization and self-sustainable programme, using every opportunity of child contact with health services for immunization, EPI being part of total comprehensive package of the child health services, presence of specially assigned, highly dedicated and professional adequate staff for EPI unit and staff in every health facility and cold store management, built-in efficient internal supervisory and monitoring system, and regular external review by WHO/UNICEF with vaccine being provided free of charge at the public health facilities.
National surveillanceTop
The national communicable disease surveillance was formally launched in Oman in March 1991 to be in conformity with the ‘communicable diseases law’ issued by the royal and ministerial decrees. The department of communicable disease surveillance and control (DCDS&C) functions as the apex body. The surveillance system ensures the collection and use of appropriate and timely data for dealing with the target priority diseases including emerging and re-emerging infections. The priority communicable diseases are grouped into ‘A’, ‘B’ and ‘C’ based on the urgency of reporting and the response. The list is dynamic. The regrouping of diseases was done in September 1993 with shifting of measles and rubella from Group ‘B’ to ‘A’ since the launching of the elimination initiative. In September 1995 ‘Viral Hemorrhagic Fever’ and in March 2003 ‘severe acute respiratory syndrome (SARS)’ and in May 2009 ‘H1N1’ were added to Group ‘A’ respectively due to their emergence and later on MERSE-CoV. The grouping of the notifiable communicable diseases was completely revised in 2005 to accommodate their current status of control/elimination, trends and changing priorities. More emphasis was placed on syndrome reporting that helps to prevent the diagnostic delays and encourages a rapid response. Currently there are 42 diseases under surveillance categorized into Group A diseases & Syndromes [5], Group B and Group C diseases [3] & Syndromes [2]. Regional epidemiologist assign at all governorates to oversee the surveillance activities [6].
Polio: In 1988, Oman achieved nearly 90% coverage of oral polio vaccine 3 (OPV3), and since 1994-95 100% coverage has been reported nationally and at provinces (Figure 1). As a result of tremendous achievement was made towards polio eradication. The last outbreak of poliomyelitis in Oman was in 1988-89 due to Type-1 polio virus resulting in 118 cases. The government then introduced five OPV doses, which were included in EPI schedule from 1989.
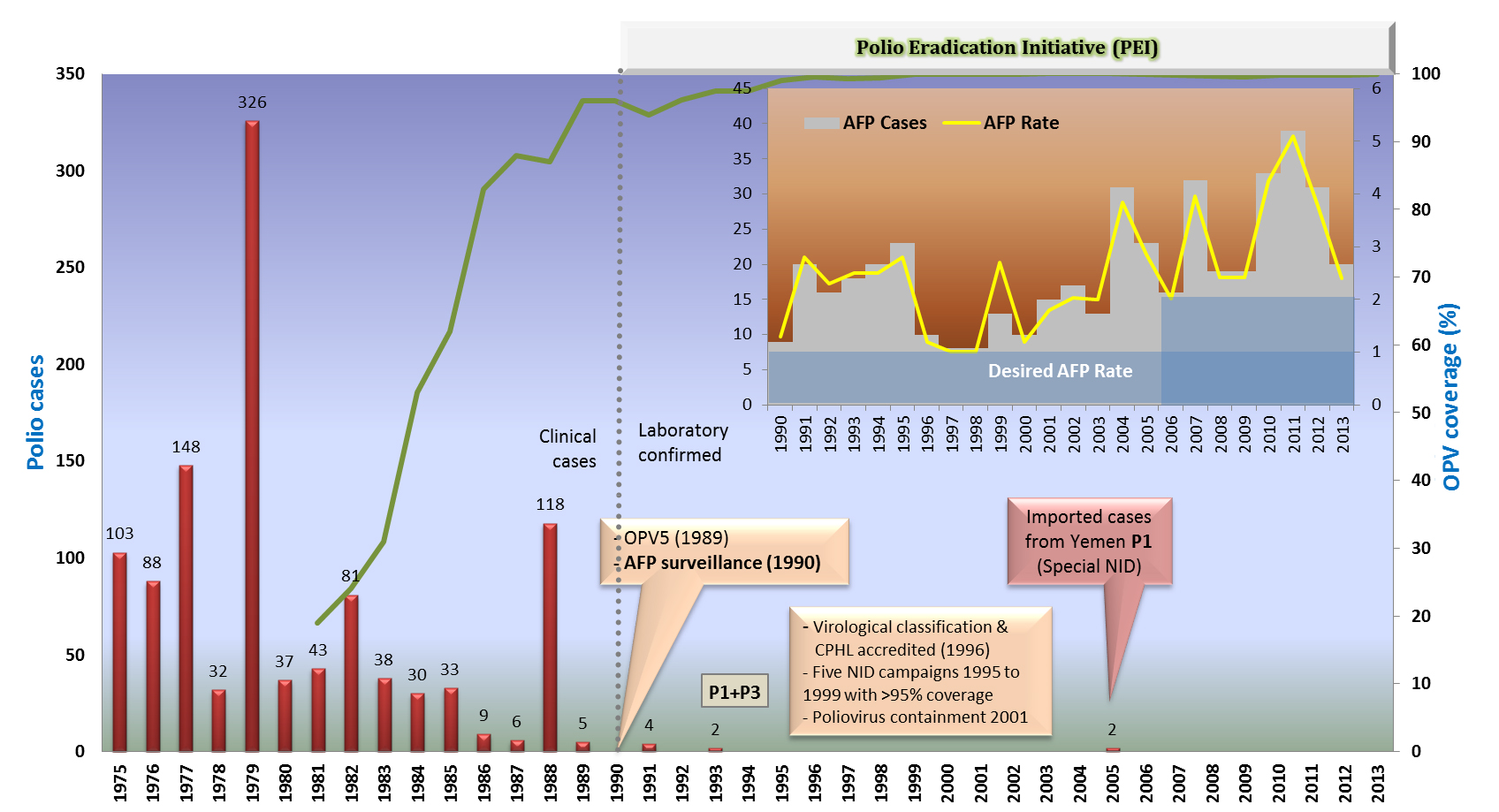
Figure 1 Polio cases and coverage (%) from 1975 to 2013, Oman.
A strong and dedicated acute flaccid paralysis (AFP) surveillance was started in 1993 and linked with immediate action and control measures. As a part of this surveillance system, 22 sentinel sites were started with weekly compulsory reporting. Since then the AFP surveillance rate has always been above the recommended rate of 2/100,000 among less than 15 years. In addition, national immunization day campaigns to ensure high coverage and quality of polio vaccinations were organized from 1995-1999. As a result of these efforts in 2005, Oman was declared to be polio free. The last 2 cases were reported in 2005 which are type-1 wild polio virus imported-related.
Diphtheria: The last case of diphtheria in Oman was reported in 1992. Due to near 99% coverage with diphtheria, tetanus and pertussis 3 (DTP3) in EPI, the elimination will be sustained hence it has been omitted from the priority list (Figure 2). Since 2003, Penta’ vaccine (DTP+Hib+HepB) has been included in EPI schedule which will replace DPT vaccine.
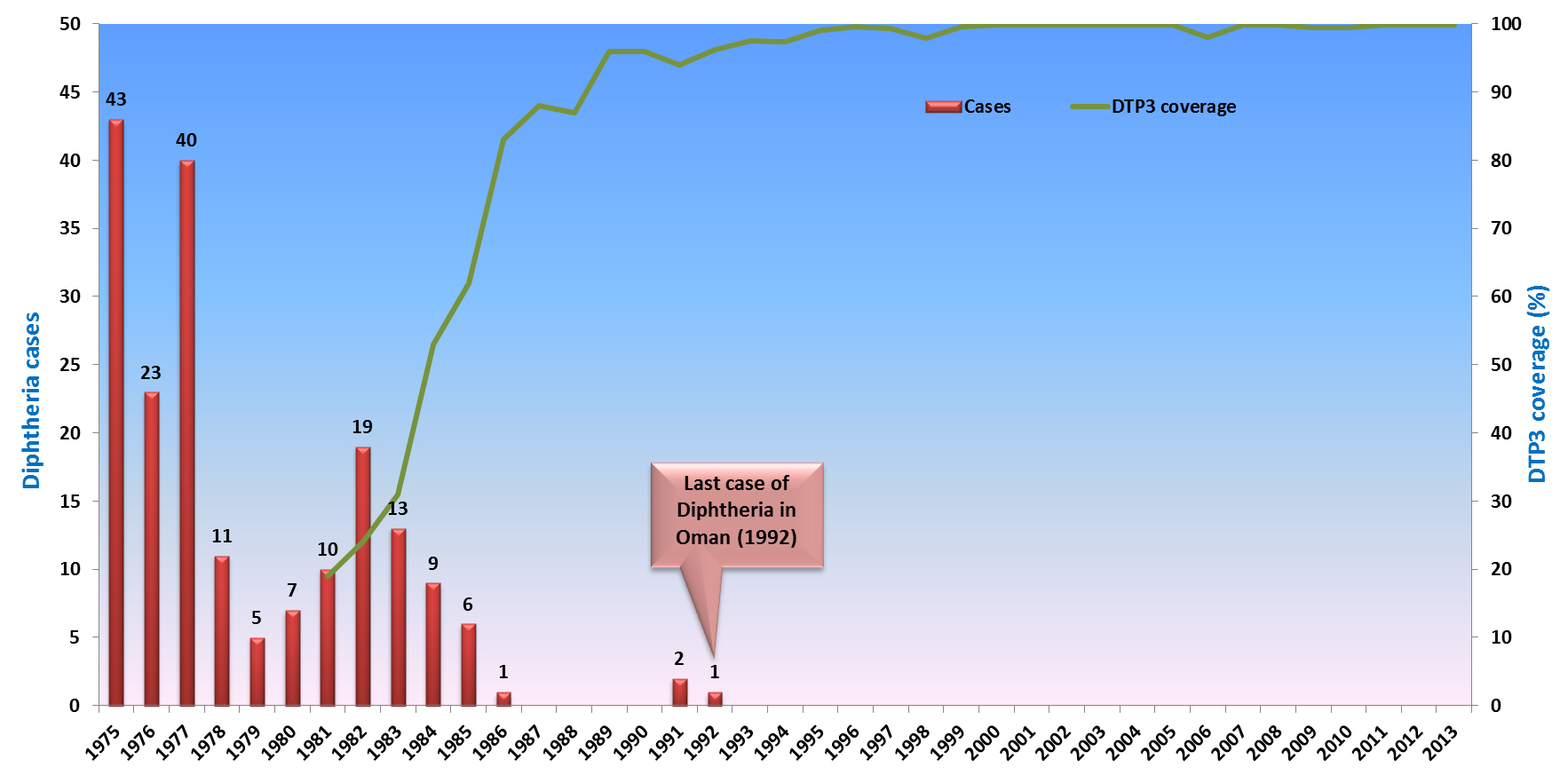
Figure 2 Diphtheria cases and coverage (%) from 1975 to 2013, Oman.
Pertussis: Pertussis is a major cause of childhood morbidity and mortality in developing countries and is caused by Bordetella pertussis, a Gram-negative bacillus. Humans are the only hosts.
In Oman, pertussis was a common childhood infection in the past. As the DTP3 coverage in the EPI maintained above 80%, the incidence dropped dramatically by late eighties (Figure 3). Due to the difficulties associated with the laboratory confirmation of pertussis only outbreaks or clusters are investigated. Majority of the sporadic cases reported are clinical. Hence the total cases reported may include cases of pertussis like illnesses of other aetiology. Subsequently, two outbreaks of pertussis were noted in some parts of the country the second being laboratory confirmed. The age distribution of the cases reported in the Sohar governorate outbreak in 1997 revealed that a large proportion of cases occurred in infants less than three months of age i.e. before the due date of DTP1. Hence, in January 1998, DTP was rescheduled in the EPI to 6 weeks, 3 months and 5 months. In January 2008, the DTP was rescheduling to be provided at 2 months, 4 months, 6 months and booster at 18 months.
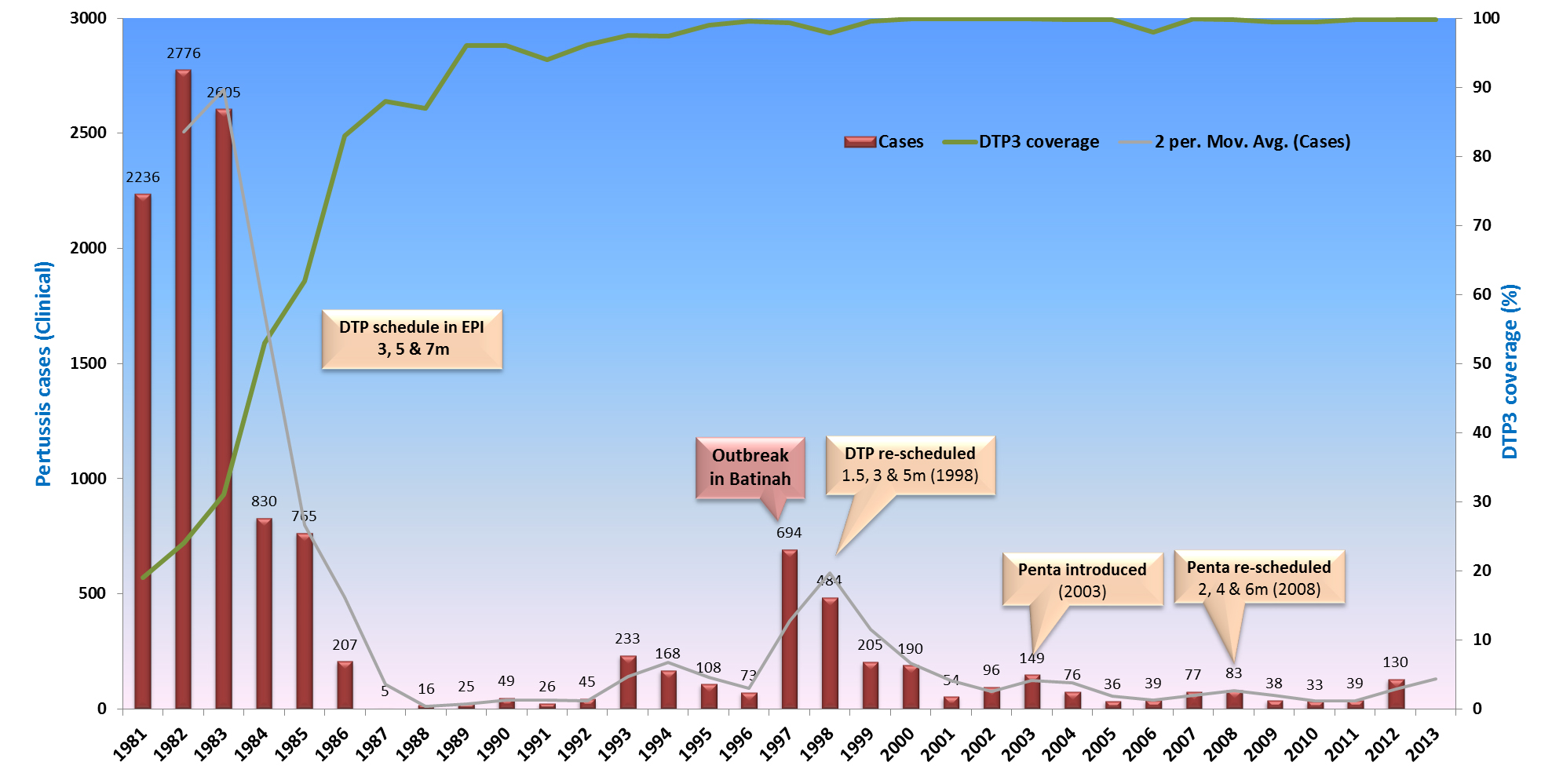
Figure 3 Pertussis cases and coverage (%) from 1981 to 2013, Oman.
Tetanus: Neonatal tetanus (NNT) elimination target based on World Health Organization (WHO) elimination criterion (i.e. less than 1 case per 1000 live births per district) has been achieved from the year 1992, hence it has been deleted from the list of priority diseases (Figure 4). Although the last case was notified in 1995 from Mussana (South Batinah governorate) still fulfilled. With the high coverage of routine and maternal tetanus toxoid 5 (TT5), the elimination is expected to remain sustained in the forthcoming years.
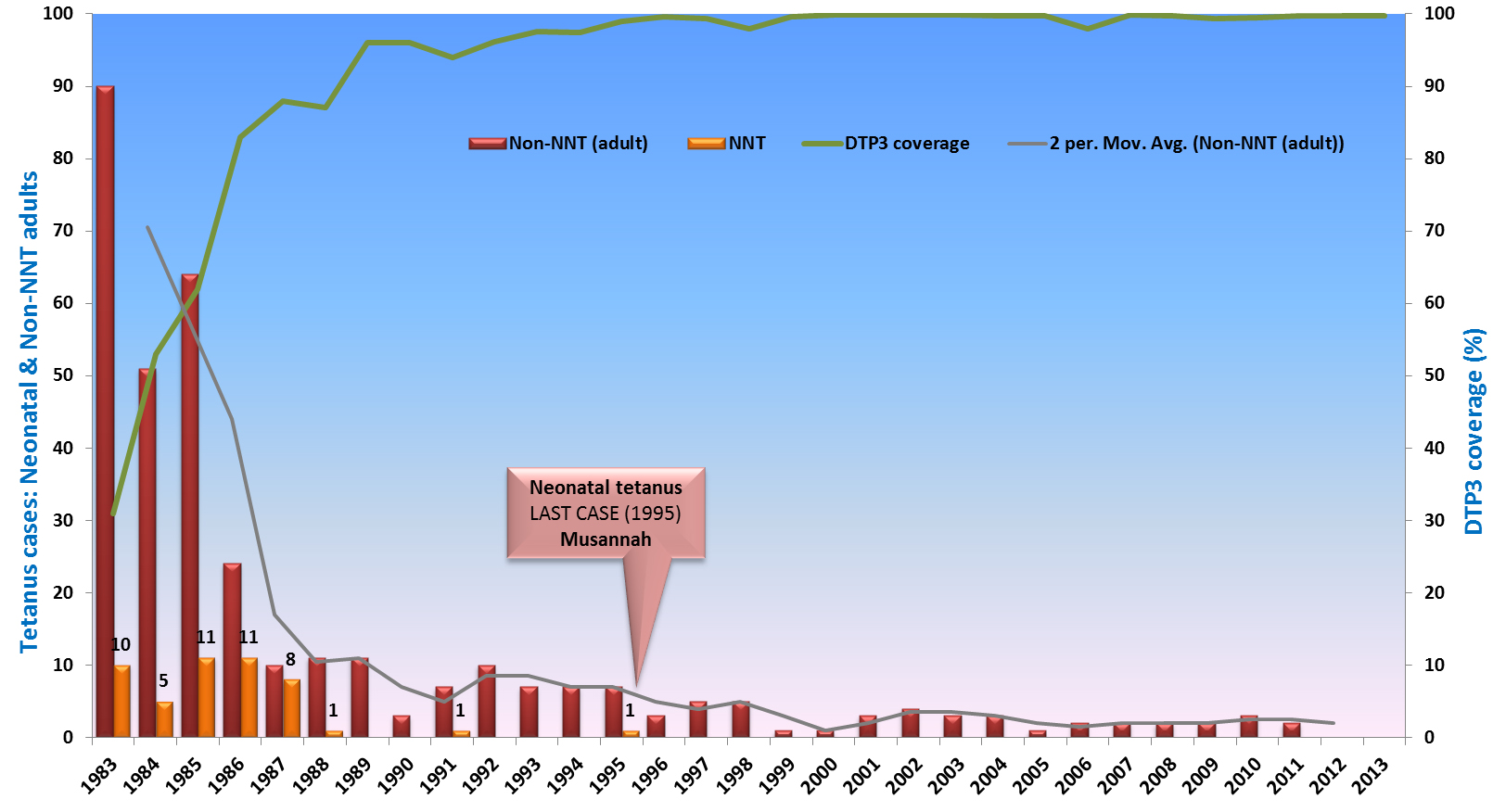
Figure 4 Neonatal and neonatal tetanus cases from 1983 to 2013, Oman.
Hepatitis B: Hepatitis B vaccination was introduced into EPI schedule from 1st August 1990 and over 97% coverage of Hepatitis B- 3 doses (HBV3) nationally and at provinces was achieved from the outset (Figure 5). Initially three doses included at birth dose, second dose at 40 days and the third at 7 months, later in 2008, it was reschedule to be at birth, 2 months and 6 months.
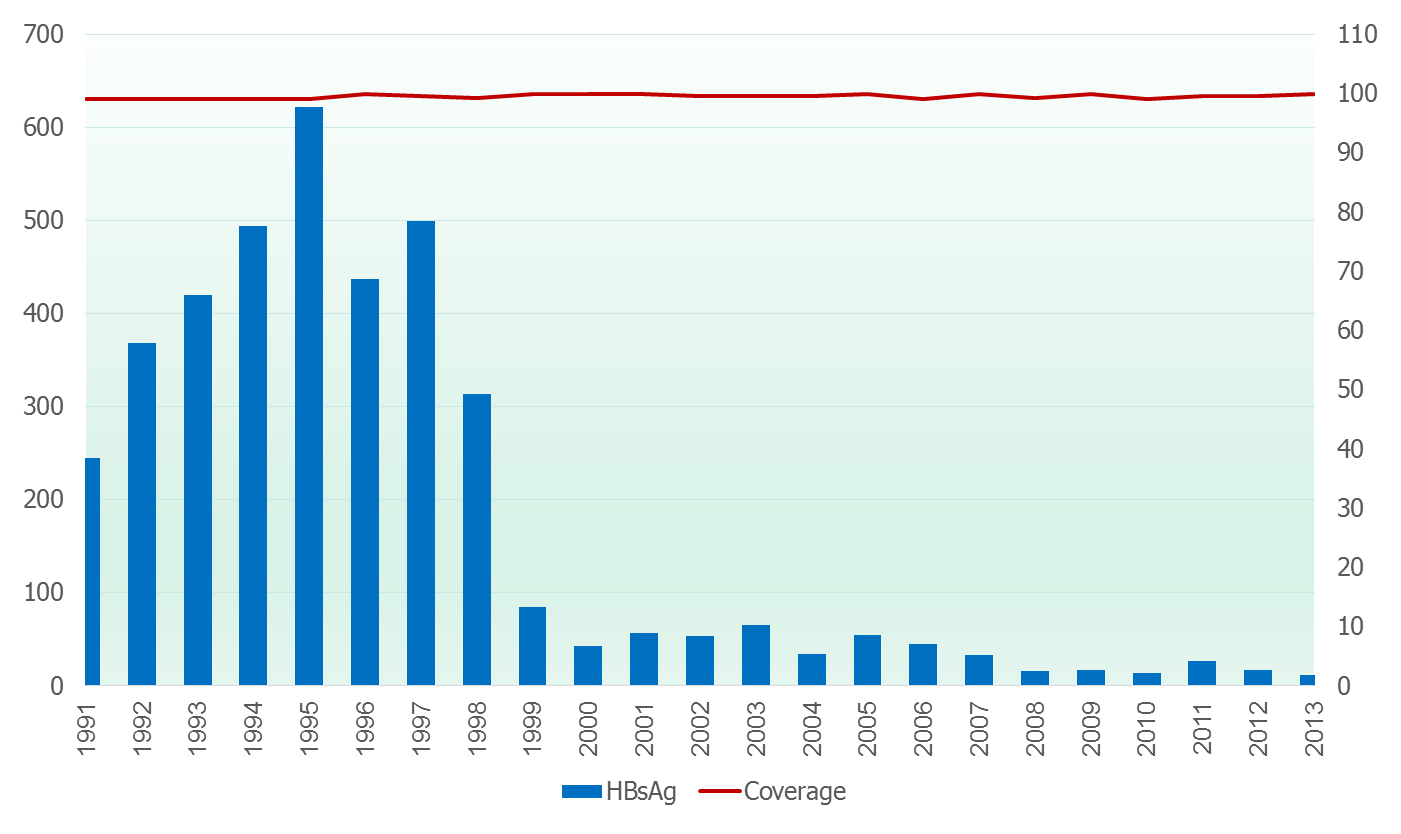
Figure 5 Incidence of viral hepatitis and hepatitis B from 1991 to 2013, Oman.
Catch-up school campaign was conducted amongst the unvaccinated adolescents (2001 to 2004) as a result by the year 2005; all persons below the age of 21 years have received the vaccination against Hepatitis B, this group comprising approximately 57% of the total population.
Currently, routine antenatal screening of mother for Hepatitis B surface antigen (HBsAg) status is NOT a policy of Ministry of Health. All family contacts of notified cases or carrier will be screened for HBsAg status and any individual who were HBsAg negative and not vaccinated, the Hepatitis B vaccine will be provided.
The same policy of contact immunization was also followed for the contacts of HBsAg positive blood donors. Mandatory screening of all blood units for surface antigen was started from 1990. Hospital wards and laboratories strictly implement precautionary measures while handling blood or body fluids and all health personnel at high risk are being immunised with Hepatitis B vaccine. All aspects of injection safety are being followed including use of disposable syringe and needles, safe disposal of waste.
Post-exposure prophylaxis using hepatitis B vaccine and/or hepatitis B immune globulin (HBIG) is used after percutaneous or mucous membrane exposures to blood that contain HBsAg such as needle-stick injury. The first phase of routine health care worker (HCW) screening and vaccination was launch in 2011.
Measles & rubella: Measles vaccine was introduced in early eighties at 9 months and the coverage has been above 90% since 1989 (Figure 6a). Rubella vaccine was introduced along with second dose of measles at 15 months as measles-rubella (MR) in 1994. Since 1994, rubella coverage has been above 95% nationally and at provinces. Introduction of rubella vaccine into EPI and later on among postpartum woman (2000) impacted on congenital rubella syndrome (CRS) (Figure 6b).
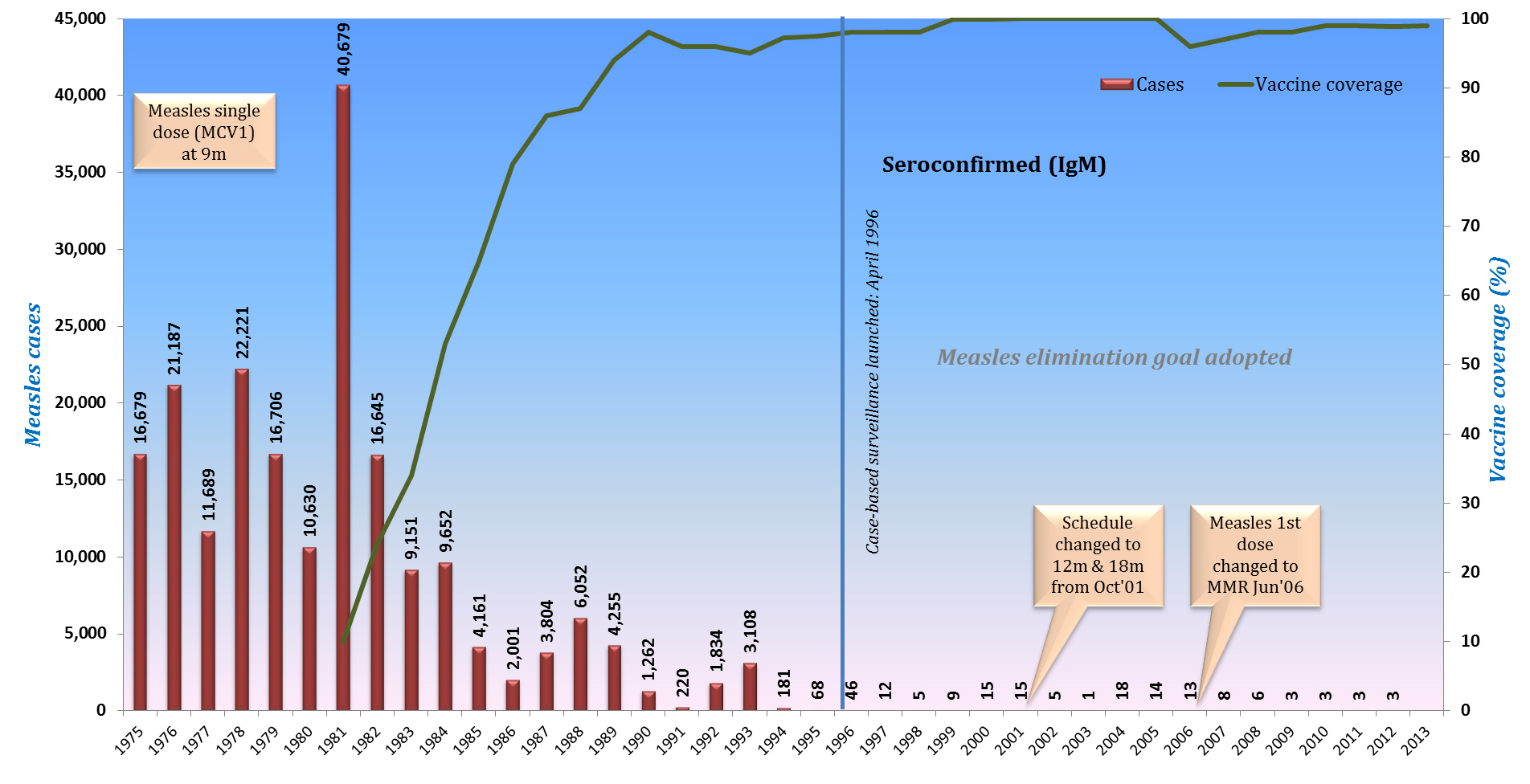
Figure 6a Measles incidence and coverage (%) from 1975 to 2013, Oman.
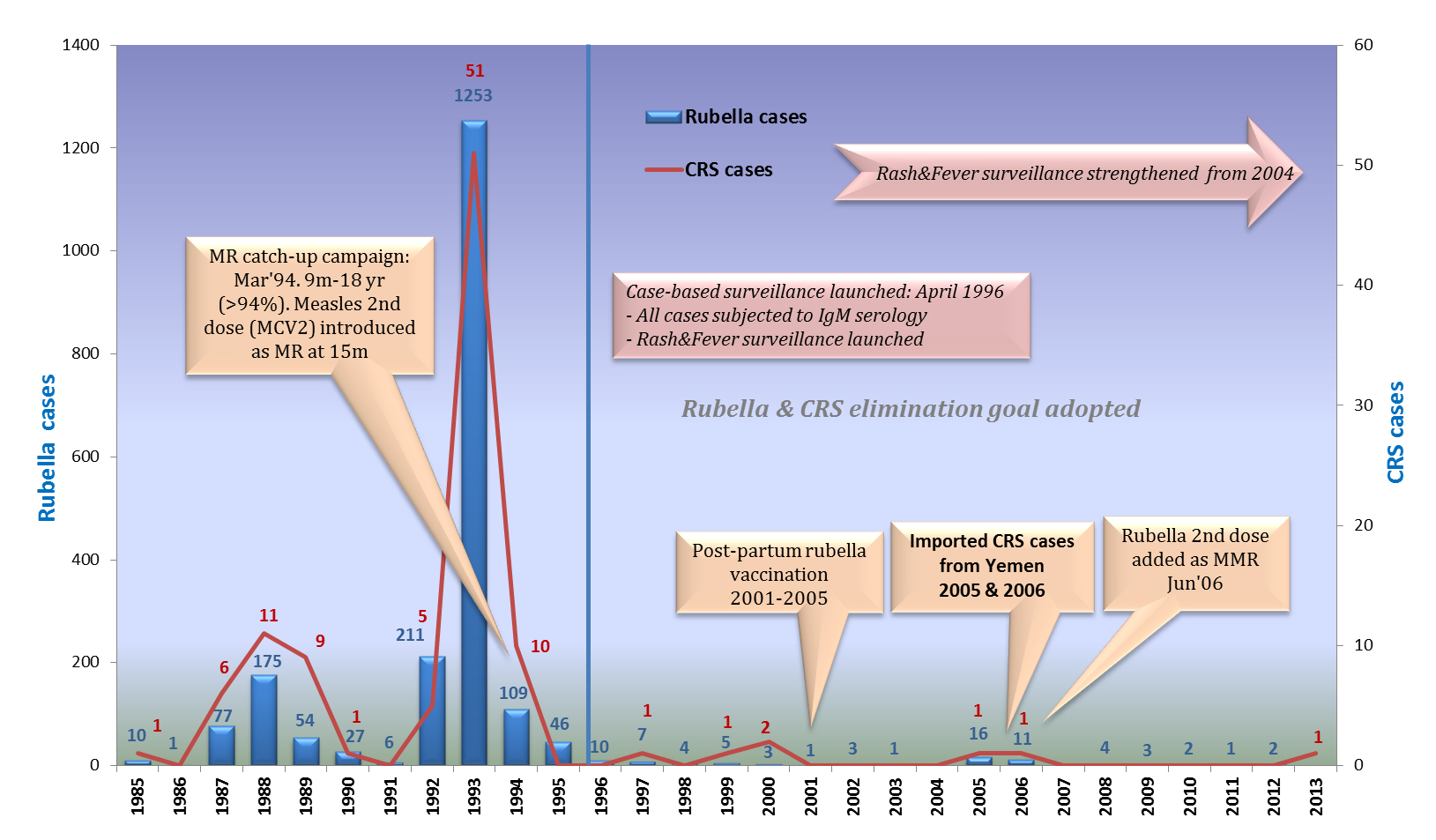
Figure 6b Rubella and CRS incidence from 1985 to 2013, Oman.
The priority status for measles and rubella was upgraded from Group B to A in 1993. A mass catch-up campaign with MR vaccine was conducted in March 1994 following the last nationwide concurrent outbreak of measles and rubella in 1992-93. The target population was 15 months to 18 years. A single dose of MR was given irrespective of the previous immunization status and in this campaign over 94% coverage was achieved [6].
Case-based rash illness surveillance was launched in April 1996. All fever-rash illness cases were subjected to serological test for measles as well as rubella (IgM ELISA). If blood sample was not taken then the case was classified as a clinical or epidemiological-linked. Urine samples were collected from all fever-rash illness cases for measles virus isolation. Fever & rash illness surveillance was further strengthened since 2005 with development of standardized case definition and laboratory investigation protocol.
Weekly negative reporting: Measles/rubella (fever-rash illness) weekly negative reporting was launched since January 1995 from the 22 sentinel sites distributed all over the country. The existing infrastructure for AFP and NNT surveillance was utilized for this purpose. The number of reporting sentinel sites was increased to 52 from January 2004.
Epidemiological investigation: All outbreaks of measles were investigated with particular reference to age, vaccination status and history of travel. Attempts were made to find out the index case and data were analysed for evaluation of the programme.
So far Oman, had successfully achieved measles/rubella elimination standards (“0” endemic cases) based on WHO elimination criteria and are reporting no endemic measles and rubella virus transmission for the last three years. Oman is experiencing a number of measles/ rubella outbreaks were all of these cases are imported or import-related with no major outbreaks indicating high population immunity.
Mumps: The mumps vaccine was introduced into the EPI programme from October 1997 as measles, mumps and rubella (MMR). The coverage has been over 99% nationally and at provinces since its introduction. Two outbreaks are evident, one in 1996 and other in 1999. Thereafter there is a continuous decline in the incidence. In 2011, 706 cases were reported as compared to about 10,000 cases in 2000 (Figure 7).
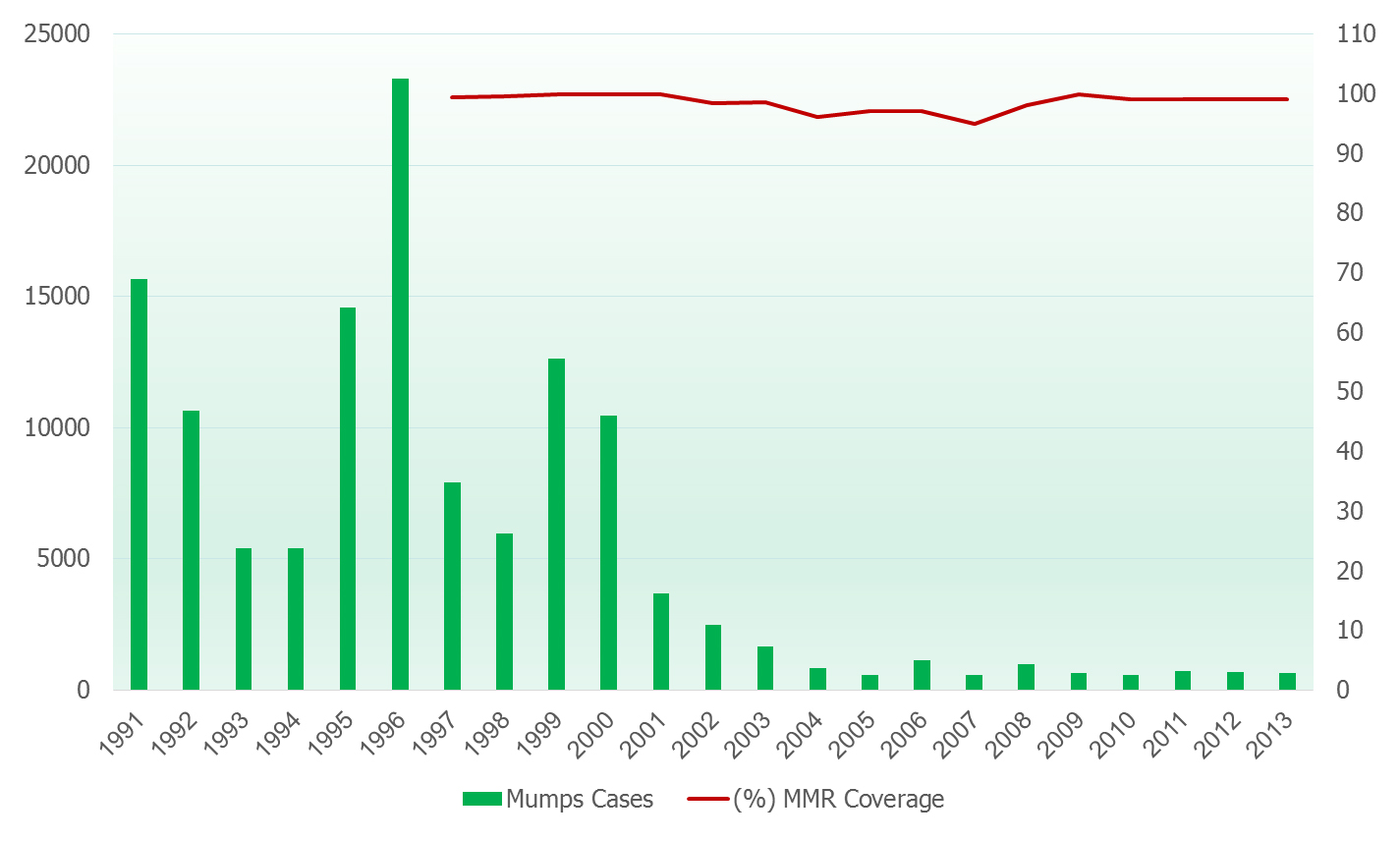
Figure 7 Incidence of mumps and coverage (%) from 1991 to 2013, Oman.
Meningococcal disease: In Oman Meningococcal meningitis is an important notifiable communicable disease (Group A, notifiable within 24 hours) due to the associated mortality and a potential risk of epidemic. Cases occur throughout the year with clustering during the period when the Hajj pilgrims return. The monthly morbidity patterns in 1988 to 1991 showed that there was an increase in the number of cases reported in the months coinciding with the return of Hajj pilgrims, who may have been carriers of Meningococcal strains and may have introduced the infection into the community. Outbreaks related to return of Hajj pilgrims in the past have been due to serogroup A. This period therefore requires close surveillance and quick action every year to prevent and control the potential outbreaks. The meningococcal vaccination is mandatory for all pilgrims for Hajj and Umra.
In 1987, outbreak the majority of cases occurred in the month of August. The prevalent serotype was Group B (WHO carrier survey December 1987). Similarly another outbreak occurred after the Hajj pilgrimage of 2000 (March/April) in which for the first time the serotype W-135 was implicated. Cases occurred in many countries and the pandemic was associated with high mortality. In Oman 28 cases were reported.
As a result of this pandemic, from the Hajj of 2001 the quadrivalent (A, C, Y, W-135) vaccine was made mandatory for the pilgrims attending Hajj & Umra. Since 2000, pandemic the disease burden has shown a decline with only 1 case reported each in 2010 and 2011 (Figure 8).
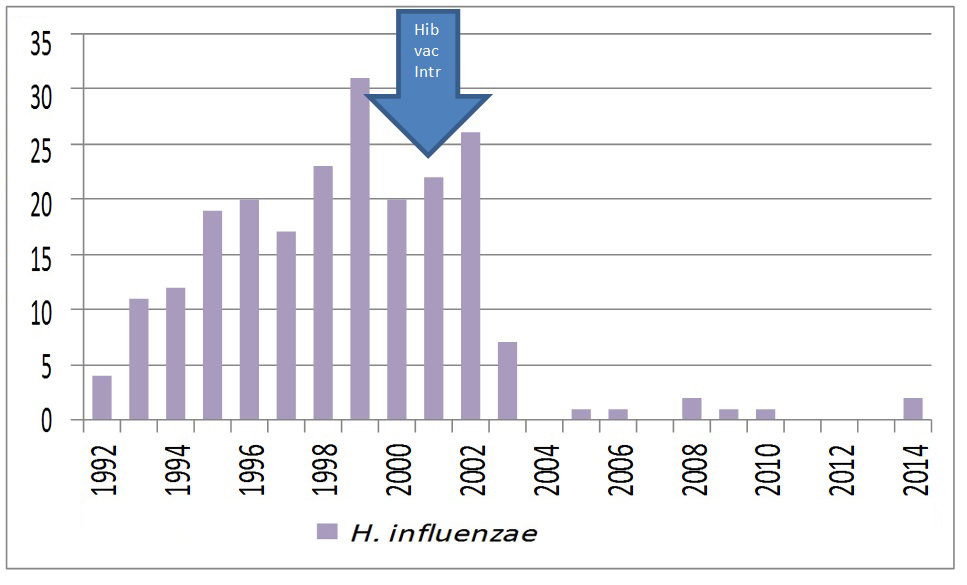
Figure 8 Haemophilus Influenzae meningitis reported from 1992 to 2014, Oman.
Hib meningitis: In Oman, Haemophilus meningitis type b was included under Group ‘B’ notifiable disease from July 1992 and to be reported within 7 days. No reliable surveillance data are available on its incidence due to the high refusal rate for lumbar puncture, pre-referral use of antibiotics and relative difficulty in isolating the organism in the laboratory. The laboratory surveillance of Hib meningitis was strengthened from the year 2000 onward. Hib vaccine has been introduced into the EPI schedule since October 2001. It was replaced with ‘Penta’ vaccine (DTPHibHepB) from July 2003. In 2005, the disease was shifted to Group A category i.e. any case was to be reported within 24 hours.
Since 2000, when about 20 cases of Hib meningitis were reported a steady decline in Hib meningitis has been seen in Oman, with 1 case reported in 2010 and no case reported in the subsequent years.
Influenza: In March 1991, influenza diseases included in Group C. However the data are unreliable due to the lack of specific case definition. In 2001, the laboratory based surveillance was initiated at four sentinel sites in Muscat and Dhofar Governorates. Isolation and typing virus is being done in collaboration with WHO-EMRO. From 2005, Influenza like illness (ILI) surveillance has been launched at the sentinel sites.
The country Influenza vaccination policy is to provide the vaccine to all high risk groups i.e. HCW, pregnant woman, immune-compromised patients and pilgrims. The uptake of seasonal influenza vaccine was always close 100% among pilgrims as it is mandatory, from 20% in 2010 to 75% in 2013 among HCW while other high risk groups are ranging between 30% and 50%. A number of strategies were adopted to enhance the uptake of seasonal influenza vaccine including availability of vaccine at all health services sites and at all times, developing of promotional materials, brochure, leaflet, posters and mouse pad, provide lectures showing the benefit of vaccine and approach in person to explain the benefit of vaccination.
National supply chain system
National primary vaccine store became the first store to meet the new WHO/UNICEF criteria of Effective Vaccine Store Management (EVSM), a built-in efficient internal supervisory and monitoring system, and regular external reviews by WHO/UNICEF with well proper storage and handling of vaccines established at all levels. In addition, guidelines were being developed to governing safety process of vaccine handling at all levels. The national supply chain management is integrated into the ‘Primary Health Care’.
DiscussionTop
A sensitive and specific surveillance system in Oman has shown a remarkable decline in the incidence of EPI target diseases. Oman has remained polio free since 1981, has had; only one case of NNT since 1992 and maintained no case of diphtheria since 1993 and has eliminated measles and rubella.
The Expanded Programme on Immunization (EPI) continues to strive to achieve and maintain high immunization coverage (>99%) for all types of vaccines nationally and at provincial levels, resulting in reduction targeting vaccine preventable diseases, especially among children indicating high population immunity.
ConclusionTop
The success of efforts against vaccine preventable diseases is mainly attributable to the successful strategic models which ensure high vaccination coverage levels, such as the strong political commitment to the EPI within MoH, the implementation of the EPI policies by the EPI static units located within the health institutions, single administrative control for EPI and supply chain management, integration of EPI services into the ‘Primary Health Care’, a decentralized and self-sustaining system, every opportunity of a child’s contact with the health services to be utilized for immunization, EPI being part of total comprehensive package of the child health services, the specially assigned. In addition to highly dedicated and professional staff for EPI unit and provision of adequate staff in every health facility and for primary vaccine store management. A built-in efficient internal supervisory and monitoring system, and regular external reviews by WHO/UNICEF with the vaccine being provided free of charge at health facilities.
Acknowledgements
We are in debt to Dr. Ali Bin Moosa, Dr. Ali Jaffer Mohammed, Dr. Ahmed Al Ghassani, Mr. Hossan Al Den, Mr. Badder Al Rawahi, Mrs. Maryam Al Shabibi, Mr. Islam Al Bulushi, Dr. Idris Al Obaidani, Mr. Arumugam Raju, Dr. Suleiman Al Busaidy, Dr. Said Al Baqlani, Dr. Shyam Bawikar, all governorate epidemiologists, Dr. Nadia Teleb, Dr. Ezzedin Mohsni, Dr. Saroj M. Sherry and Akash Malik, for their vision and support.
Conflict of interest
The authors declare no conflict of interest.
ReferencesTop
[1] World Health Organization (WHO) (2014) Global immunization data. Geneva: WHO. Available July 2014. Article
[2] World Health Organization (WHO) (2013) The global vaccine action plan 2011–2020. Geneva: WHO. Available October 2014. Website
[3] Ministry of Health (2012) Communicable Disease Surveillance & Control Expanded programme on immunization, Sultanate of Oman. Available September 2014. Website
[4] The Oman World Health Survey 2008 (OWHS 2008), page 108. Available October 2014. Website
[5] Ministry of health (1995) Community Health & Disease Surveillance Newsletter, Sultanate of Oman, 2(3).
[6] Ministry of Health (2002) Manual on expanded program on immunization, Department of Surveillance & Disease Control, Sultanate of Oman. Available July 2014. Article



