Journal of Modern Human Pathology
An International Peer-Reviewed Open Access Journal
ISSN 2397-6845


- Download PDF
- |
- Download Citation
- |
- Email a Colleague
- |
- Share:
-
- Tweet
-

Journal of Modern Human Pathology
Volume 3, Issue 4, May 2018, Pages 12–14
Case reportOpen Access
Cul-de-sac splenosis - An unusual location
- 1 Departments of Pathology and Laboratory Medicine, The University of Kansas Medical Center, Kansas City, Kansas 66160, USA
- 2 Departments of Obstetrics and Gynecology, The University of Kansas Medical Center, Kansas City, Kansas 66160, USA
*Corresponding author: OssamaTawfik, MD, PhD., Professor, Department of Pathology and Laboratory Medicine, The University of Kansas Medical Center, Kansas City, Kansas 66160, USA. Tel.: (913) 588-1185; E-mail: otawfik@kumc.edu
Received 20 February 2018 Revised 10 April 2018 Accepted 20 April 2018 Published 04 May 2018
DOI: http://dx.doi.org/10.14312/2397-6845.2018-4
Copyright: © 2018 Rivas E, et al. Published by NobleResearch Publishers. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
AbstractTop
We present a unique case of splenosis in a 36-year-old female in the posterior cul-de-sac of the lower pelvis, and to our knowledge, has never previously been reported. Her splenosis persisted for years, mis-diagnosed as a gynecologic condition. The differential diagnosis, clinical, radiological and histologic findings are discussed along with review of the literature.
Keywords: differential diagnosis; laparoscopy; splenic tissue; pelvic splenosis; cul-de-sac
IntroductionTop
Splenosis is a rare benign condition of auto transplanted splenic tissue in other compartments of the body. It commonly occurs after splenic rupture due to trauma or surgery [1]. The majority of the cases are asymptomatic and incidentally found on routine imaging. Commonly, splenosis is seen in the peritoneum, omentum, and mesentery. Pelvic splenosis makes up a minority portion in the literature [2, 3]. Pelvic splenosis in women can be challenging to diagnose due to the numerous gynecological benign and malignant conditions that are more commonly encountered in these patients [4, 6].
Case summaryTop
A 36-year-old female presented to our institution with a complaint of pain with ovulation for the past six months. The patient had a history of thyroid cancer and an unremarkable gynecological history. She denied having dysmenorrhea or pain with bowel movements. Outside imaging was done and two masses where discovered in the posterior cul-de-sac along with subserosal fibroids. On ultrasound the masses were isoechoic and measured 3.0 and 1.3 cm in greatest dimension. On MRI the lesions were mildly increased T1 and slightly decreased T2 and measured 2.0 × 2.3 × 1.7 cm and 1.3 × 1.4 × 1.2 cm. Endometriosis was a possible diagnosis and a plan was discussed with the patient of observation with interval imaging versus diagnostic laparoscopy with possible biopsy. The patient consented to have a diagnostic laparoscopy.
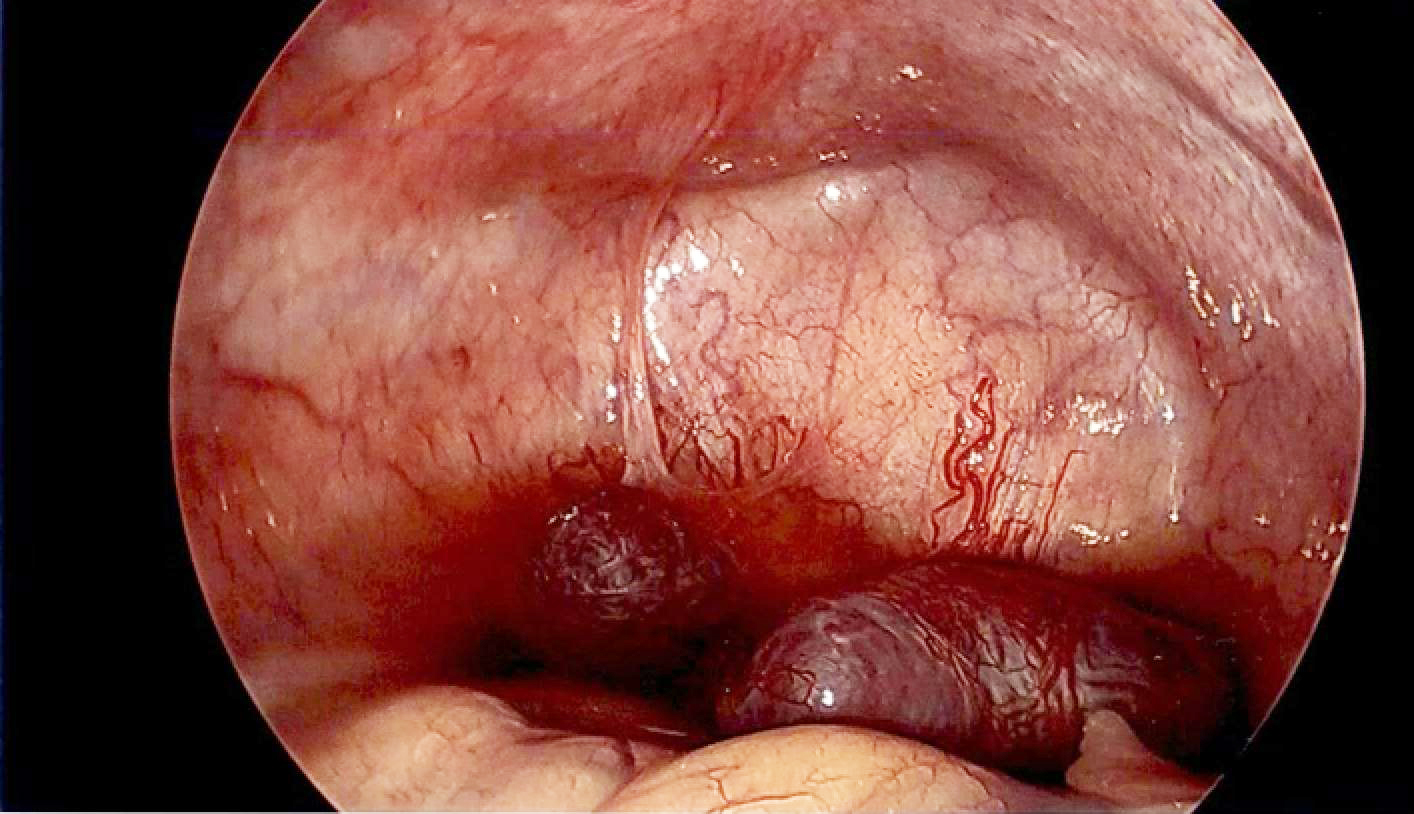
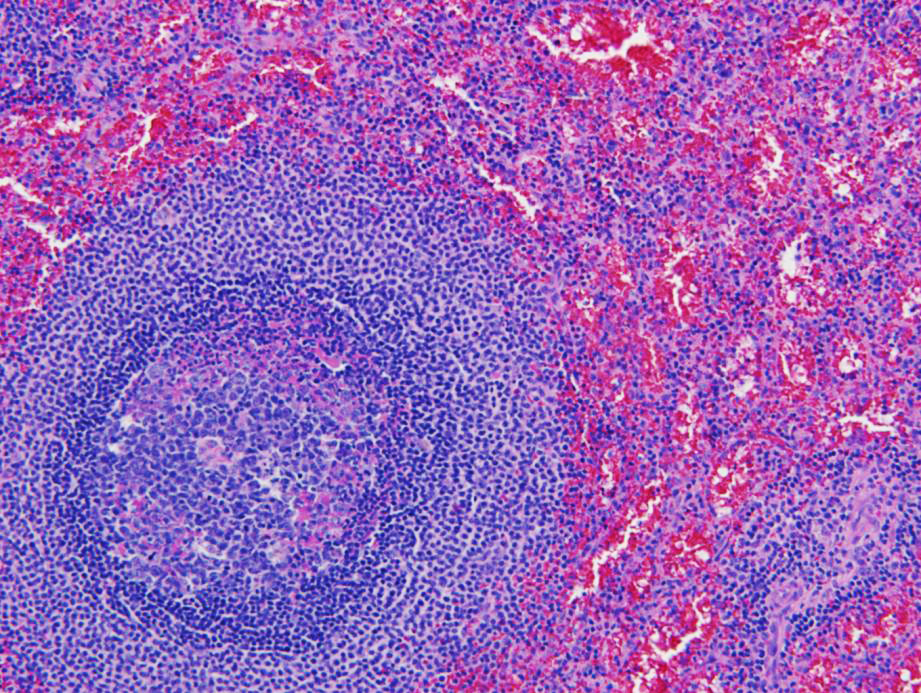
During the operation three red-brown masses were identified. One was at the anterior surface of the uterus and measured 1.0 cm. The other two masses were located in the posterior cul-de-sac and measured 3.0 × 2.0 cm and 2.0 × 2.0 cm (Figure 1). The posterior masses were attached to the peritoneum in the cul-de-sac just overlying the rectum leaching their blood supply from the peritoneum. Prior to resection, pelvic washings were collected. These three masses were easily resected utilizing gentle traction and a bipolar vessel sealing device and were removed through a tissue retrieval pouch. There was minimal bleeding at the site of resection. Histopathologic evaluation showed benign splenic tissue consistent with pelvic splenosis (Figure 2).
After discussing the pathology results with the clinician, it was questioned whether the patient had a traumatic event in the past that caused her spleen to rupture. It was confirmed that the patient was involved in a serious automobile accident 12 years before that caused her spleen to rupture. The additional medical history of traumatic splenic rupture supported the diagnosis of splenosis.
DiscussionTop
Splenosis is a rare, benign condition of heterotopic auto transplantation of splenic tissue into other compartments of the body. It has been estimated to develop in up to 67% of patients with traumatic splenic rupture [1, 4]. The pathogenesis of splenosis is primarily due to the rupture of the splenic capsule and seeding of splenic tissue in nearby body cavities [1, 4, 5]. The average interval between trauma and the detection of the splenic tissue was reported to be at least 10 years [6]. Fewer than 100 cases of splenosis have been reported in the literature [3]. The most common location of splenosis is found in the abdominal cavity, primarily within the peritoneal cavity, omentum and/or mesentry [2]. Pelvic and/or gynecological splenosis has rarely been reported. Uncommon locations like the thoracic cavity, subcutaneous tissue and the brain have also been encountered [3, 7]. The mechanism of intra thoracic and subcutaneous splenic tissue is when trauma causes a path of entry [7]. However, it must be assumed that a hematogenous spread has occurred for cerebral splenosis [5, 7].
Splenosis is commonly asymptomatic and is incidentally found on routine imaging or during surgery [1]. Splenosis at a first glance can be concerning for a neoplastic process [5]. Since splenosis mimics metastases it is important to keep in mind in patients with cancer to avoid unnecessary surgery or chemotherapy [3]. If it occurs in the pelvis, pelvic pain, dysmenorrhea or other gynecologic symptoms may occur [8]. Pelvic splenosis can be especially hard to diagnosis because of the many gynecological conditions such as leiomyomas, endometriosis and other neoplastic processes [1, 4]. Splenosis and endometriosis share diffuse peritoneal spread and differ in intraperitoneal adhesions splenosis [9]. One would have a very high index of suspicion for reaching the accurate diagnosis to avoid unnecessary therapies. Indeed, such was the case with our patient whose splenosis condition was assumed to have been uterine leiomyomas for years. Splenosis could also be confused with accessory spleens [4]. However, in contrast to an accessory spleen, splenosis derives its blood supply from nearby vessels [1]. Furthermore accessory spleens are usually found near the splenopancreatic or gastrosplenic ligament [10].
Multiple radiologic techniques could be used to accurately diagnose splenosis. Technetium 99 is the most sensitive and specific diagnostic technique for splenosis as it detects small nodules that could be missed on MRI [1, 4]. If large enough, the masses have similar attenuation on CT as splenic tissue [4]. On unenhanced sequences splenosis implants show homogenous hypointensity on T1 weighted images and hyperintensity on T2 weighted images [1]. SPIO can be used to diagnose splenosis as it is taken up by reticuloendothelial cells [1]. Single-photon emission CT (SPECT) may be helpful in diagnosing splenosis because it provides accurate 3D images and more detailed functional information [11]. Splenosis parasitizes blood from surrounding tissue and creates a rich vascular network; significant blood can be lost during surgery [7]. Serpiginous enhancement on the arterial phase is virtually diagnostic, but is hard to see in small nodules [1].
Grossly splenosis nodules differ from malignant lesions in color and consistency, but remain to be challenging with other benign conditions [9]. A recent review of the literature discussed that splenosis has different microanatomy with less white pulp and does not have the same phagocytic capacity as normal spleen tissue [12]. Histologically splenosis nodules have a distorted architecture with no hilum, poorly formed capsule and tissues of variable size [8]. It has also been shown that splenosis nodules are immunologically active; potentially providing benefit for the patient [4]. The absence of siderocytes on a peripheral smear can help diagnose splenosis [9]. Patients who have undergone splenectomy due to a hematological disease, recurrence of the hematological disease can point to splenosis [9].
Symptomatic splenosis nodules are most often treated by surgical removal. Recently non-invasive approaches to pelvic splenosis are advocated [9]. In 1995 Higgins and Crain reported the first successful laparoscopic removal of pelvic splenosis [13].
ConclusionTop
We present a unique case of splenosis in the lower pelvis within the posterior cul-de-sac which masqurated for years as a gynecological condition. Following removal of the splenosis nodules further investigation revealed traumatic splenic rupture secondary to a serious automobile accident 12 years prior was obtained. This case highlights the value of a thorough clinical history in facilitating accurate diagnosis. A high index of suspicion is recommended for accurate diagnosis to avoid unnecessary or delayed treatment.
Conflict of interest
None of the authors have a conflict of interest either financial or of personal nature that is connected to the submitted manuscript.
Funding
There is source of funding for the data presented in this case report.
ReferencesTop
[1]Lameiras R, Matos AP, Luz C, Palas J, Ramalho M. Pelvic splenosis–a very unusual location. BJR Case Rep. 2017; 2:20160026.Article
[2]Parnell BA, Palmer CB, Forstein DA. Pelvic splenosis presenting as posterior cervical mass. South Med J. 2010; 103(4): 388–389.Article Pubmed
[3]Metindir J, Mersin HH, Bulut MZ. Pelvic splenosis mimicking ovarian metastasis of breast carcinoma: A case report. J Turk GerGynecol Assoc. 2011; 12(2):130–132.Article Pubmed
[4]Gerber D, Frey MK, Caputo TA. Pelvic splenosis misdiagnosed as a uterine sarcoma. GynecolOncol Rep. 2015; 12:1–2.Article Pubmed
[5]Lake ST, Johnson PT, Kawamoto S, Hruban RH, Fishman EK. CT of splenosis: Patterns and pitfalls. Am J Roentgenol.2012; 199(6):W686–W693.Article Pubmed
[6]Anrique D, Anton A, Kruger K, Niedobitek-Kreuter G, Ebert AD. Splenosis: An uncommon differential diagnosis in Gynecology. J Minim Invasive Gynecol. 2013; 20(5):708–709.Article Pubmed
[7]Talati H, Radhi J. Ovarian splenosis: a case report. Case Rep Med. 2010; 2010:472162.Article Pubmed
[8]Park SY, Kim JY, Lee JH, Choi JS, Ko JH, et al. Laparoscopic management of pelvic splenosis. ObstetGynecol Sci. 2014; 57(1):89–91.Article Pubmed
[9]Segev Y, Lavie O, Goldberg Y, Kaufman Y, Peerl G, et al. Pelvic splenosis mimicking an ovarian mass: non-invasive approach. Isr Med Assoc J. 2007; 9(11):819–820.Article Pubmed
[10]Tsitouridis I, Michaelides M, Sotiriadis C, Arvaniti M. CT and MRI of intraperitoneal splenosis. DiagnIntervRadiol. 2010; 16(2):145–149.Article Pubmed
[11]Sarraf KM, Abdalla M, Al-Omari O, Sarraf MG. Diagnostic difficulties of pelvic splenosis: case report. Ultrasound Obstet Gynecol. 2006; 27(2):220–221.Article Pubmed
[12]Duivenvoorden R, de Sonnaville JJ, van Muiswinkel JM. An accidental finding of multiple abdominal and pelvic tumors.Neth J Med. 2013; 71(7):371–375.Article Pubmed
[13]Higgins RV, Crain JL. Laparoscopic removal of pelvic splenosis: A case report. J Reprod Med. 1995; 40(2):140–142.Pubmed



