Journal of Modern Human Pathology
An International Peer-Reviewed Open Access Journal
ISSN 2397-6845


- Download PDF
- |
- Download Citation
- |
- Email a Colleague
- |
- Share:
-
- Tweet
-

Journal of Modern Human Pathology
Volume 3, Issue 5, October 2018, Pages 15–17
Case reportOpen Access
Ectopic liver tissue in the fundus of the stomach: A case report
- 1 Department of Pathology, University of Illinois at Chicago, 840 S Wood Street, CSN 130, Chicago, IL 60612, USA
*Corresponding author: Erica Vormittag-Nocito, Department of Pathology, University of Illinois at Chicago, 840 S Wood Street, CSN 130, Chicago, IL 60612, USA. Tel.: 1-561-601-0614; E-mail: Evormi2@uic.edu
Received 09 August 18 2018 Revised 05 September 2018 Accepted 15 September 2018 Published 20 September 2018
DOI: http://dx.doi.org/10.14312/2397-6845.2018-5
Copyright: © 2018 Vormittag-Nocito E, et al. Published by NobleResearch Publishers. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
AbstractTop
Ectopic liver tissue is a rare entity that most commonly occurs on the gallbladder wall. Rare case reports within the literature have documented cases of ectopic liver within the pylorus of the stomach. Therefore, we present a case of a patient with ectopic liver tissue occurring in the gastric fundus wall.
Keywords: ectopic liver tissue; stomach wall; fundus
IntroductionTop
Ectopic liver (EL) is a rare entity with an incidence of 0.24% - 0.48% and prevalence of 0.47% [1]. EL is defined as normal liver tissue located outside the liver without a connection to the normal liver. If a connection exists, it is considered an accessory lobe. Most instances of EL are asymptomatic and only discovered sporadically during surgery or autopsy. Symptomatic cases are due to torsion, necrosis, rupture, malignant transformation, or mass effect compression [2]. In the present report, we describe a 73-year-old female with a submucosal gastric mass identified as EL.
Case descriptionTop
A 73-year-old female with past medical history of iron deficiency anemia, multiple myeloma, and atherosclerosis presented to the Gastroenterology clinic at the University of Illinois Hospital and Health Sciences System in Chicago, Illinois for endoscopic ultrasound examination for a previously visualized submucosal fundic mass and a pancreatic cyst. Her previous stay at a hospital for iron deficiency anemia included an esophagogastroduodenoscopy (EGD) which identified a submucosal mass within the fundus of the stomach without overlying mucosal ulceration or evidence of bleeding. A biopsy of the submucosal lesion of the stomach wall was attempted, but no submucosal tissue was present in this biopsy. A follow-up computed tomography (CT) scan was performed and the mass in the fundus was well circumscribed, located completely within the wall of the stomach and measured 1.9 cm in greatest dimension. Additionally, a pancreatic cyst within the pancreatic head was identified measuring 1.6 cm in greatest dimension.
During the endoscopic ultrasound the cyst within the pancreatic head was identified, measuring 1.6 × 1.6 cm. It did not appear to connect to the pancreatic duct. It consisted of a single compartment without septae and no associated mass lesion was identified. A small amount of fluid was collected, and concentrations of carcinoembryonic antigen (CEA) and amylase were measured. The level of CEA and amylase in the collected fluid was 6.7 ng/mL and 7124 U/L, respectively. These values were normal for pancreatic fluid. Unfortunately, no cytology was performed on this fluid.
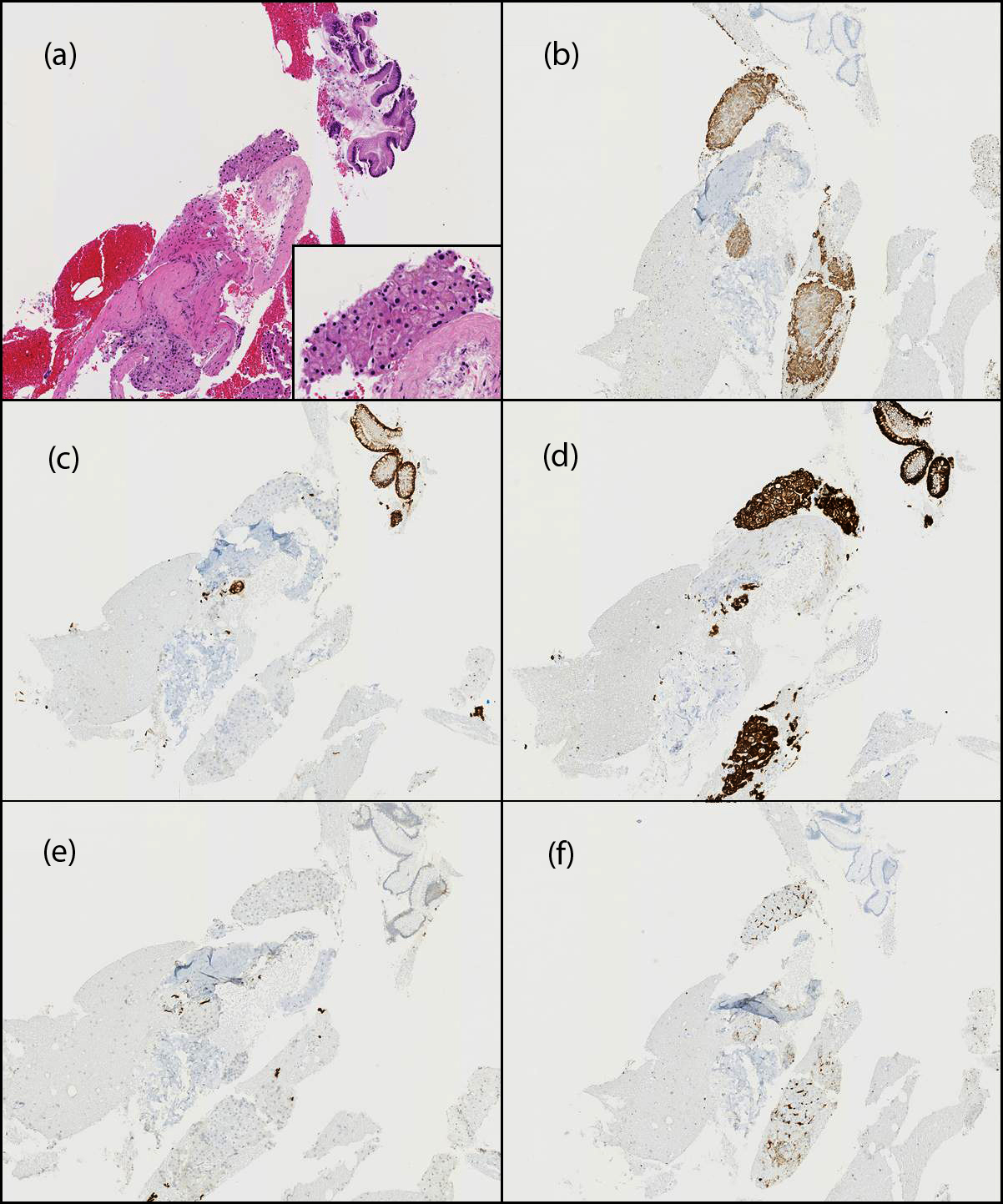
The lesion in the fundus of the stomach was then identified by endoscopic ultrasound. This examination showed its hypoechoic character and dimensions of 1.2 × 1.2 cm. Fine needle aspirations (FNA) were performed and a core biopsy were performed. The cytology of the passes showed spindled cells that were not lesional tissue; meanwhile, the core biopsy showed scant benign gastric mucosa with small aggregates of polygonal cells with abundant eosinophilic cytoplasm and granule formation (Figure 1). The aggregate cells were stained by immunohistochemistry. Single labeling revealed positive reactions of these cells for HepPar1 (a hepatocytic marker) and CAM5.2 (epithelial marker) and negative for CK19 and CK7 (markers of hepatocellular carcinoma) as well as p63 (epithelial marker), S100 (melanoma marker) and CD163 (macrophage marker). These results confirm the presence of ectopic hepatocytes within the fundus of gastric wall.
DiscussionTop
EL parenchyma is a rare occurrence with less than 100 cases reported in the English literature. Earlier studies found that 0.05% of 5500 autopsies [3] and 0.7% [4] patients during laparoscopic surgery showed incidental EL. Currently, the most common site of incidental finding of EL is on the wall of the gallbladder [1, 5]. Moreover, EL has also been identified in the thorax, lung, pancreas, umbilicus, adrenals, pylorus, inferior vena cava and within congenital abdominal wall anomalies [2, 6, 7].
The cause of EL parenchyma is still unknown, but many theories have been developed based on the stages of liver embryogenesis. EL may develop as a migration error or displacement of part of the pars hepatica, a dorsal budding event before the closure of the pleuroperitoneal cavity (the potential source of thorax deposits), trapping of mesenchymal cells that later differentiate into hepatocytes, entrapment of cell nests within the foregut after closure of the diaphragm, and atrophy or regression of the connection of a liver bud from the rest of the liver [3, 7-10].
Only three cases have been reported of EL tissue within the gastric wall [11, 12]. Two of these cases reported by Arakawa et al. have shown transformation to hepatocellular carcinoma. Interestingly, these cases of carcinoma development within the EL do not show lesions within normal liver parenchyma suggesting increased carcinogenesis within ectopic tissue. Thus, we can suppose that abnormal flow of metabolites may induce a chemical carcinogenic effect on EL but further studies are necessary to confirm this hypothesis.
Our patient was discovered to have a submucosal mass within the gastric wall of the fundus. To our knowledge, no other case report has identified EL within the fundus of the stomach, as the other cases within the literature were located in the pylorus. It should be noted that various neoplasms were considered in the clinical differential diagnosis for this patient including gastrointestinal stromal tumor, plasmacytoma associated with multiple myeloma, gastric carcinoma and possible metastasis of unknown primary. While EL parenchyma was overlooked clinically due to its rare occurrence. In this case, the diagnosis of benign EL tissue prompted no additional clinical intervention, despite the known increased risk of developing hepatocellular carcinoma in this location.
ConclusionTop
Ectopic liver tissue is a rare occurrence in the thoracic and abdominal cavity. When identifying a well circumscribed submucosal mass within the gastrointestinal tract, EL tissue should also be taken into account in the differential diagnosis. To our knowledge, this is the first report of EL tissue occurring in the gastric fundus.
Conflicts of interest
Authors declare no conflicts of interest.
ReferencesTop
[1]Mani VR, Farooq MS, Sovi U, Kalabin A, Rajabalan AS, et al. Case report of ectopic liver on gallbladder serosa with a brief review of the literature. Case Rep Surg. 2016; 2016:7273801.Article Pubmed
[2]Bal A, Yilmaz S, Yavas BD, Ozdemir C, Ozsoy M, et al. A rare condition: Ectopic liver tissue with its unique blood supply encountered during laparoscopic cholecyctectomy. Int J Surg Case Rep. 2015; 9:47–50.Article Pubmed
[3]Watanabe M, Matsura T, Takatori Y, Ueki K, Kobatake T, et al. Five cases of ectopic liver and a case of accessory lobe of the liver. Endoscopy. 1989; 21(1):39–42.Article Pubmed
[4]Soto S, Wantanabe M, Nagasawa S, Niigaki M, Sakai S, et al. Laparoscopic observations of congenital anomalies of the liver. Gastrointest Endosc. 1998; 47(2):136–140.Article Pubmed
[5]Topcu R, Erkent M, Kendirci M, Sahiner IT. Ectopic liver tissue on the gallbladder wall: A case report and literature review. Indian Journal of Research. 2018; 7(2):582–583.Article
[6]Barazza G, Adler DG, Factor RE. An unexpected diagnosis of ectopic liver diagnosed by fine needle aspiration. Cytojournal. 2016; 13:29.Article Pubmed
[7]Park WH, Choi SO, Lee SS, Randolph JG. Ectopic umbilical liver in conjunction with biliary atresia: Uncommon association. J of Pediatric Surgery. 1991; 26(2):219–222.Article Pubmed
[8]Abhilash S, Karthik K, Singh KL, Ranita Devi S, Moirangthem GS. Ectopic Liver in gallbladder: A case report. J Evol Med Dent Sci. 2015; 4(9):1574–1576.Article
[9]Hamdani SD, Baron RL. Ectopic liver simulating a mass in the gallbladder wall: Imaging findings. AJR Am J Roentgenol. 1994; 162(3):647–648.Article Pubmed
[10]Tejada E, Danielson C. Ectopic or heterotopic liver (choristoma) associated with the gallbladder. Arch Pathol Lab Med. 1989; 113(8):950–952.Pubmed
[11]Arakawa M, Kimura Y, Sakata K, Kubo Y, Fukushima T, et al. Propensity of ectopic liver to hepatocarcinogenesis: Case reports and a review of the literature. Hepatology. 1999; 29(1):57–61.Article Pubmed
[12]Huang W, Xu X, Li T, Zhang H, Chen Y, et al. Ectopic liver tissue in stomach paries: A case report. Int J Clin Exp Pathol. 2015; 8(9):11704–11707.Article Pubmed



