Journal of Radiology and Imaging
An International Peer-Reviewed Open Access Journal
ISSN 2399-8172


- Download PDF
- |
- Download Citation
- |
- Email a Colleague
- |
- Share:
-
- Tweet
-

Journal of Radiology and Imaging
Volume 2, Issue 2, February 2017, Pages 6–10
Original researchOpen Access
Reduction of radiation dose in adult CT-guided musculoskeletal procedures
- 1 Department of Imaging, Cedars-Sinai Medical Center, Los Angeles, California, USA
*Corresponding author: Charles Rawson, Department of Imaging, Cedars-Sinai Medical Center, 8700 Beverly Blvd Ste M335, Los Angeles, CA 90048, USA. Tel.: (310)423-2723; Fax: (310)423-8335; E-mail: rawson.charles@gmail.com
Received 16 November 2016 Revised 18 January 2017 Accepted 25 January 2017 Published 29 January 2017
DOI: http://dx.doi.org/10.14312/10.14312/2399-8172.2017-2
Copyright: © 2017 Rawson C, et al. Published by NobleResearch Publishers. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
AbstractTop
Objective: We examine the effect of manually reducing CT scanner tube voltage (kVp) and current (mA) on patient radiation dose and procedural success during CT-guided musculoskeletal procedures on adults. We hypothesize that patient radiation dose can be reduced while maintaining procedural success. Materials and methods: This project was performed as an operational test of change. Scanner kVp and mA were manually reduced during CT-guided musculoskeletal procedures over a 6-month period (n = 20). Bilateral cases served as their own controls. The remaining control cases were obtained by retrospective review of our picture archiving and communication system. Default scanner voltage and current were recorded for all dose reduced cases. Using an experimentally derived formula, we calculated what the total exam DLP would have been had the default settings been used. In addition, a 32 cm acrylic body phantom was scanned using the recorded default and reduced settings for the dose reduced cases. Results: Radiation dose reduction for all procedures vs. control cases was statistically significant at 68% (p < 0.001). Average dose reduction for all procedures vs. calculated normal dose was statistically significant at 69% (p < 0.001). Average radiation dose for all cases using phantom scans was statistically significant at 72% (p < 0.001). All procedures were successful. Conclusion: Our study shows that significant reduction in radiation dose without reduction in procedural accuracy can be achieved by simply lowering the CT scanner voltage and current from their default settings.
Keywords: radiation dose; CT-guided procedure; musculoskeletal procedure
IntroductionTop
While computerized tomography (CT) guided procedures represent a small portion of total CT examinations, their radiation dose can be significant to both patients and imaging personnel. For many musculoskeletal lesions, especially those which are deep or purely osseous, CT is the modality of choice for image guidance [1, 2].
Image guided percutaneous biopsy offers multiple benefits over open biopsy including minimal invasiveness with decreased morbidity and recovery time, ability to direct needle to areas most likely to yield diagnostic specimens, high accuracy, and lower cost [1]. Dupuy et al reported 93% accuracy for CT-guided needle biopsy of musculoskeletal neoplasms [3].
With increased public scrutiny on radiation risks, optimizing and balancing image quality while keeping radiation dose as low as reasonably achievable (ALARA) is vital [4]. Artner et al. have demonstrated the effectiveness of CT dose reduction strategies during CT-guided spinal, periradicular, and sacroiliac joint injections [5-7]. However, to the authors’ knowledge, no prior studies have examined the effectiveness of CT dose reduction over a wide spectrum of CT-guided musculoskeletal procedures in the adult population. The purpose of the study is to examine the effect of manually reducing CT scanner tube voltage (kVp) and current (mA) on patient radiation dose and procedural effectiveness during CT-guided musculoskeletal procedures on adults.
Materials and methodsTop
This project was performed as an operational test of change. The IRB approval was obtained. The procedures were performed by a single board certified musculoskeletal radiologist who manually reduced tube voltage (kVp) and current (mA) from the CT scanner's default settings during 20 CT-guided musculoskeletal procedures performed on adults over a 6-month period from 9/2013 to 3/2014. The practitioner reduced the settings taking into account body part, patient body habitus, and patient age. Tube voltage was reduced by an average of 25% for helical scans and by 9% for snapshot CT snapshot mode. Tube current was reduced by an average of 38% for helical scans and by 35% for CT snapshot mode. Default settings, adjusted settings, and dose length product (DLP) were recorded. We chose the total DLP to estimate the total surrogate radiation to the patient as we felt this was a better representation than a dose index such as CTDIvol as it takes into account the entire length of the patient scanned rather than a single slice and sums the radiation doses from the initial helical scan with the snapshot mode portion. All cases were performed on a 16-slice multidetector CT (Lightspeed RT 16; General Electric Medical Systems, Waukesha, WI, USA) with CT snapshot mode (GE SmartView). Radiation doses were calculated assuming a standard 32 cm acrylic body phantom.
Three bilateral cases (2 subtalar injections and 1 ankle injection) served as their own controls, as one side was performed with default tube voltage and current while the other side was performed with reduced current and voltage. The remaining 17 control cases were obtained by searching the picture archiving and communication system (PACS) for CT-guided musculoskeletal procedures matched for body part and procedure performed over the year prior to the dose reduction cases (i.e. sacroiliac joint injection vs. sacroiliac joint injection, femur biopsy vs. femur biopsy, etc.).
Our department’s workflow for CT-guided MSK procedures begins with placing a skin marker over the region of interest. Anteroposterior and lateral scout views of the region of interest are then obtained and the position of the skin marker is adjusted if needed. Using these scouts and prior diagnostic studies the radiologist selects the cranial and caudal boundaries for a helical CT to just cover the lesion/joint of interest. A skin entry point is selected. CT snapshot mode is used for needle guidance, during which three adjacent CT slice still images are obtained when the foot pedal is pressed.
The default scanner voltage and current were recorded for all dose reduced cases. For the same collimation (3i) and scan length, the following relationship was experimentally derived for our procedural CT scanner (kVp ranged from 80 to 120):
![]() . We calculated what the total exam DLP would have been had the default settings been used. In addition, a 32 cm acrylic body phantom was scanned using the default and reduced settings which had been recorded for the dose reduced cases.
. We calculated what the total exam DLP would have been had the default settings been used. In addition, a 32 cm acrylic body phantom was scanned using the default and reduced settings which had been recorded for the dose reduced cases.
Procedures were comprised of three types: Joint injection/aspiration, bone biopsy, and soft tissue biopsy/drainage. Biopsies were considered successful if the sample was diagnostic on pathology report. Joint injection/aspiration was considered successful if the needle tip was imaged within the joint space. A post hoc calculation of statistical power for a decrease in procedural success rate from 99% to 95% during dose reduced procedures is 0.18.
Statistical significance was calculated with SPSS software (version 22.0; IBM, Armonk, NY, USA) utilizing the Mann-Whitney U test.
ResultsTop
A total of 20 CT-guided MSK procedures (6 joint aspirations/injections, 10 bone biopsies, and 4 soft tissue biopsies/drainages) were performed. Table 1 summarizes the radiation doses and radiation dose reduction of each group, including calculated DLPs and scans of phantoms. Table 2 summarizes the contribution of the helical scan and snapshot mode to the total radiation dose for reduced dose cases. Table 3 summarizes the default protocol and dose reduced CT scanner settings which were used.
| Case Type | Protocol | n | Mean radiation dose (DLP in mGy-cm) | 95% CI (DLP in mGy-cm) | Average dose reduction (%) | p-value |
| All cases | Reduced dose | 20 | 111.76 | 68.98 - 154.55 | 68 | < 0.001 |
| Normal dose | 20 | 351.15 | 264.00 - 438.13 | |||
| Calculated normal dose | Normal dose | 20 | 375.27 | 246.28 - 504.25 | 69 | <0.001 |
| Phantom cases - all | Reduced dose | 20 | 95.57 | 61.47 - 129.67 | 72 | < 0.001 |
| Normal dose | 20 | 303.91 | 225.66 - 382.17 | |||
| Joint aspirations/injections | Reduced dose | 6 | 117.26 | -52.54 - 287.06 | 71 | 0.041 |
| Normal dose | 6 | 342.31 | 29.7 - 654.92 | |||
| Bone biopsies | Reduced dose | 10 | 104.04 | 71.21 - 136.83 | 68 | < 0.001 |
| Normal dose | 10 | 336.41 | 246.81 - 426.01 | |||
| Soft tissue biopsies/drainages | Reduced dose | 4 | 122.83 | 42.07 - 203.59 | 65 | 0.029 |
| Normal dose | 4 | 401.27 | 178.52 - 624.01 |
| Dose reduced case | Helical DLP (mGy-cm) | Snapshot mode DLP (mGy-cm) | Total DLP (mGy-cm) |
| 1 | 112.28 | 10.04 | 122.32 |
| 2 | 50.85 | 13.3 | 64.15 |
| 3 | 27.7 | 0.85 | 28.55 |
| 4 | 27.57 | 1.92 | 29.49 |
| 5 | 19.2 | 1.44 | 20.64 |
| 6 | 418.33 | 20.08 | 438.41 |
| 7 | 112.28 | 14.07 | 126.35 |
| 8 | 101.05 | 16.08 | 117.13 |
| 9 | 74.87 | 1.00 | 75.87 |
| 10 | 59.03 | 6.36 | 65.39 |
| 11 | 80.05 | 26.88 | 106.93 |
| 12 | 59.03 | 11.59 | 70.62 |
| 13 | 139.69 | 67.82 | 207.51 |
| 14 | 119.39 | 15.08 | 134.47 |
| 15 | 63.21 | 22.26 | 85.47 |
| 16 | 46.49 | 4.15 | 50.64 |
| 17 | 53.23 | 0.8 | 54.03 |
| 18 | 118.41 | 1.59 | 120.00 |
| 19 | 164.85 | 8.31 | 173.16 |
| 20 | 139.13 | 5.00 | 144.13 |
| Average percentage of total DLP | 89.00 | 11.00 |
| Procedure | Helical CT | Snapshot CT | ||||||
| Dose Reduced | Protocol | Dose Reduced | Protocol | |||||
| kVp | mA | kVp | mA | kVp | mA | kVp | mA | |
| SI joint injection | 100 | 200 | 120 | 280 | 100 | 40 | 100 | 60 |
| SI joint injection | 80 | 180 | 120 | 280 | 80 | 40 | 120 | 60 |
| Subtalar injection | 80 | 17 | 120 | 44 | 80 | 30 | 80 | 80 |
| Subtalar injection | 80 | 70 | 120 | 100 | 80 | 40 | 120 | 60 |
| Subtalar injection | 80 | 60 | 120 | 100 | 80 | 20 | 80 | 40 |
| Hip aspiration | 100 | 360 | 140 | 440 | 100 | 40 | 120 | 60 |
| biopsy iliac | 100 | 200 | 120 | 440 | 100 | 40 | 120 | 60 |
| biopsy iliac | 100 | 160 | 120 | 280 | 100 | 40 | 120 | 40 |
| biopsy iliac | 80 | 340 | 120 | 440 | 100 | 15 | 120 | 25 |
| biopsy iliac | 80 | 220 | 120 | 280 | 80 | 40 | 80 | 60 |
| biopsy sacrum | 100 | 200 | 120 | 280 | 100 | 20 | 120 | 25 |
| biopsy ischium | 80 | 220 | 120 | 300 | 120 | 25 | 80 | 25 |
| biopsy acetabulum | 100 | 280 | 120 | 440 | 100 | 30 | 100 | 60 |
| biopsy femur | 100 | 18 | 120 | 80 | 80 | 30 | 80 | 80 |
| biopsy femur | 80 | 280 | 120 | 440 | 80 | 120 | 80 | 280 |
| biopsy tibia | 100 | 14 | 120 | 80 | 100 | 25 | 120 | 60 |
| biopsy thigh soft tissue | 80 | 120 | 120 | 200 | 80 | 15 | 120 | 25 |
| biopsy thigh soft tissue | 80 | 130 | 120 | 165 | 80 | 60 | 80 | 80 |
| biopsy chest wall | 100 | 300 | 120 | 440 | 80 | 40 | 100 | 60 |
| pelvic abscess drainage | 120 | 200 | 120 | 280 | 120 | 30 | 120 | 30 |
Of note, the radiation dose reduction for all procedures vs. control cases was statistically significant at 68% (p < 0.001). Average dose reduction for all cases vs. calculated normal dose was statistically significant at 69% (p < 0.001). Average radiation dose for all cases using phantom scans was statistically significant at 72% (p < 0.001). When compared to control cases, statistically significant radiation dose reduction was also observed for each type of procedure; 71% (p = 0.041) for joint aspirations/injections, 68% (p < 0.001) for bone biopsies, and 65% (p = 0.029) for soft tissues biopsies/drainages.
Before reducing the CT tube current and voltage we recorded the default current and voltage for each case. Using these default settings we were able to calculate what the DLP would have been had the current and voltage not been reduced. When compared to these calculated DLPs, our dose reduction was 69%. We also scanned a 32 cm acrylic body phantom using both default and reduced settings which had been recorded for reduced dose cases. The results for these phantom scans showed a 72% reduction in DLP, which agrees well with the 69% reduction we demonstrated vs. calculated radiation doses, and 68% reduction vs. control cases. Given the small number of cases, we thought these added points of comparison may be useful.
All procedures were successful with 13 biopsies being diagnostic, six joint aspirations/injections having the needle tip imaged within the joint space, and one pelvic abscess drainage having successful drain placement with return of purulent material. No procedural complications were observed.
DiscussionTop
When compared with control cases, we achieved a statistically significant average radiation dose reduction of 68% without loss of procedural success. This is less than the 87% dose reduction demonstrated by Patel et al for musculoskeletal biopsies in the pediatric population and less than the 85-94% dose reductions achieved by Artner et al. for spinal, periradicular, and sacroiliac joint injections [2, 5-7]. As we experienced no loss in procedural success, this suggests that we may have room to further decrease radiation doses. It should be noted that for the purposes of consistency, once a reduced scanner voltage and current were selected, they were not changed (either lowered if image quality was more than sufficient or increased if image quality was too poor). We did not encounter any instances where image quality was too poor to safely perform the procedure; however this remains a possibility in practice. Practitioners should feel free to increase and decrease scanner current and voltage to achieve sufficient image quality to safely perform the procedure at hand with the extent of radiation dose reduction ultimately limited by the image quality with which an individual practitioner feels comfortable.
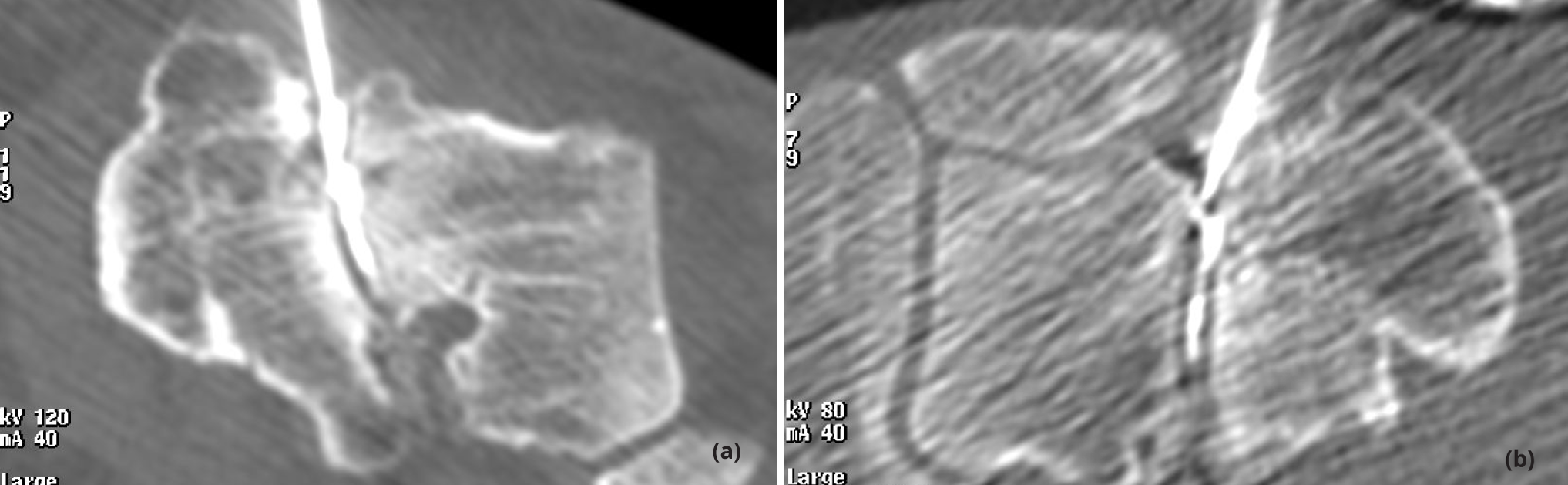
With decreased radiation dose comes decreased image quality, as demonstrated by Figure 1. This is offset by a couple of factors. Firstly, there is nearly always prior diagnostic quality imaging available for comparison. Second, a diagnostic quality image is not necessary to visualize high contrast structures such as needles, joint spaces, and osseous lesions. Only enough radiation should be used to visualize structures that need to be seen during the procedure at hand, that is the ALARA principle [4].
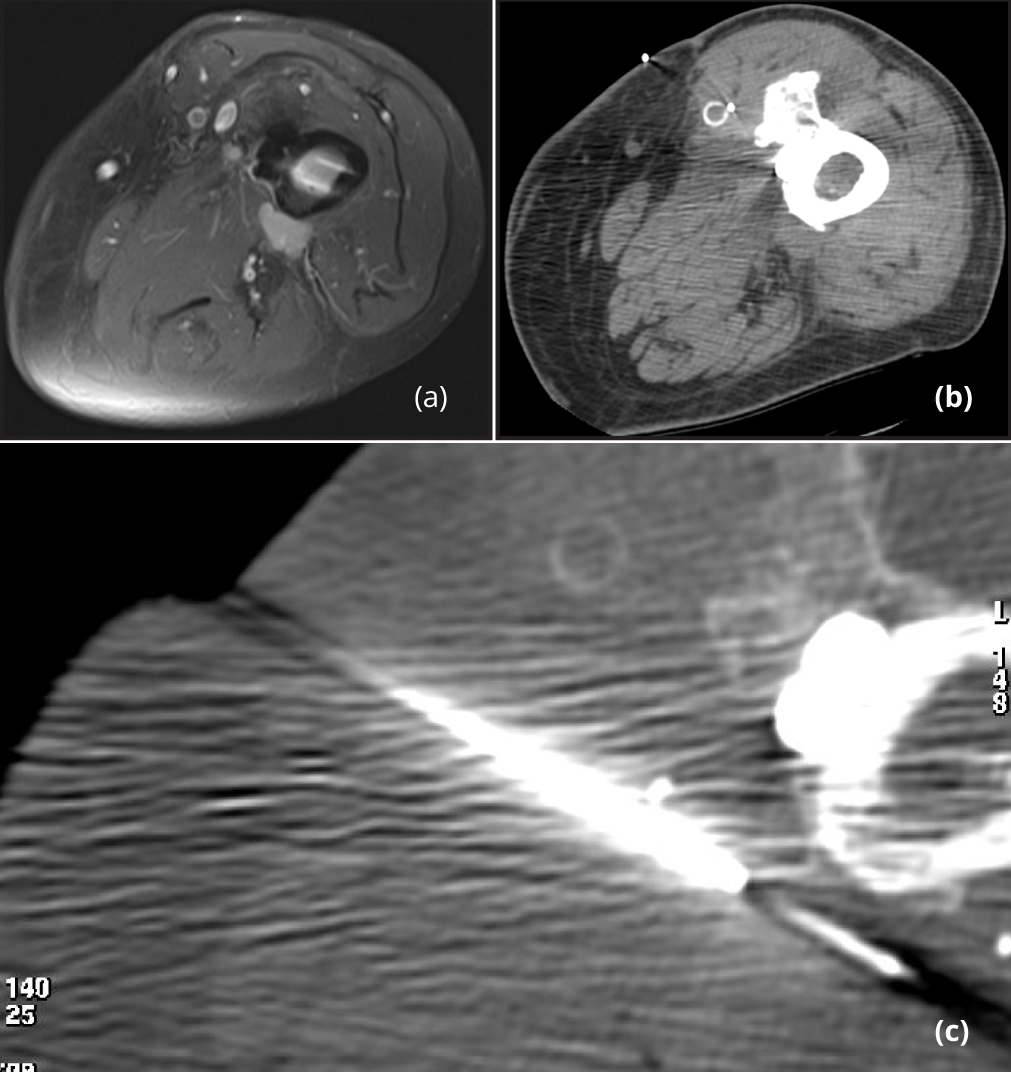
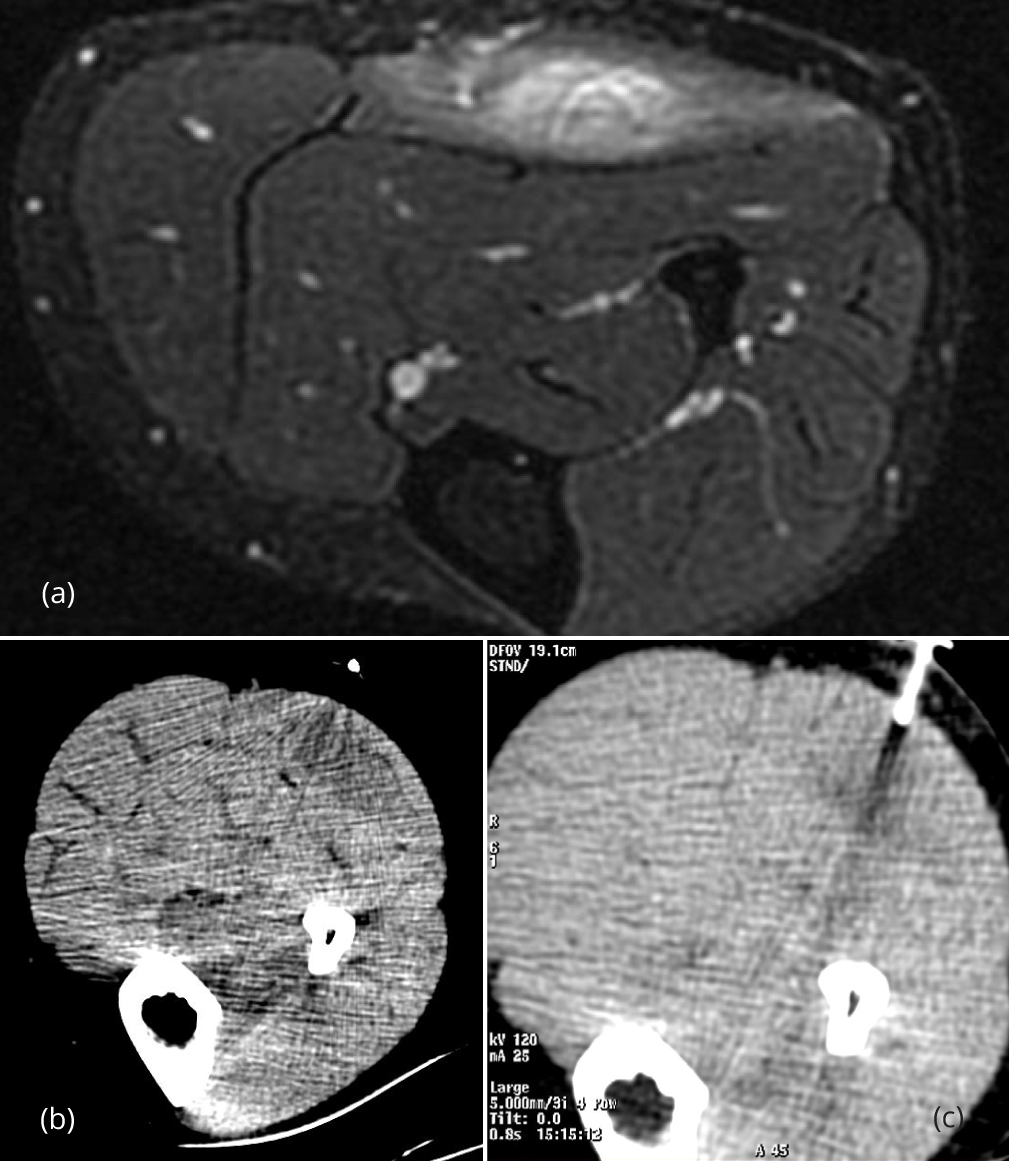
In cases where lesions are close to sensitive structures, such as arteries and nerves, dose reduction may not be appropriate as image quality needs to be maintained to visualize and avoid these critical structures. One such case is demonstrated by Figure 2. Ill-defined soft tissue lesions which are difficult to visualize on CT are also not good candidates for radiation dose reduction as they may be impossible to see with decreased image quality. In such cases, radiation may be avoided all together by utilizing ultrasound or MRI guidance. Figures 3 demonstrate such a case. In our experience, sternal biopsies are also not good candidates for dose reduction.
As shown in Table 2, the initial helical scan contributes 89% of the total radiation dose; with the snapshot mode contributing the remaining 11%. This suggests that the area for greatest potential dose reduction lies not only with decreasing current and voltage during this initial helical scan, but by judiciously limiting the length of this helical scan to only the area of interest. Likewise, smaller radiation dose savings can be accomplished by doing the same with during the snapshot mode. This is the reason we chose to represent total patient radiation dose with DLP rather than CTDIvol as it takes into account not only the radiation dose to an individual slice of the patient, but to how much of the patient has been irradiated. If the CTDIvol for the helical and snapshot mode portions of the exam were equal, the DLP for the helical portion will nearly always be higher than the snapshot mode due to the sheer number of slices imaged.
The major limitation to this study is its small population size. A post hoc statistical power calculation suggests that we would only detect a decrease in procedural success from 99% to 95% (i.e. a five-fold increase in failure rate) during dose reduced procedures 18% of the time; however radiation dose reductions for all groups of procedures were significant. Control procedures are limited as well as no two CT-guided procedures are exactly alike. Bilateral cases served as their own controls and are as close to true controls as possible. However, comparisons between procedures done on different people are limited by different scan lengths, patient body habitus, and bone mineral density. As all dose reductions were done manually with varying degrees of reduction based on region of interest, patient body habitus, and patient age, repeatability of this study is limited. However, even if this study is not exactly repeatable, it serves to illustrate that a practitioner can simply manually lower current and voltage from their default settings and obtain significant radiation dose reduction to the patient. The degree to which a radiologist is willing to decrease radiation dose, and therefore image quality, will vary based on the individual. The DLPs we observed were slightly different between real dose reduced cases and phantom cases performed at the same settings. This may have been due to automatic current modulation, but it raises the point that calculation of exact radiation doses is not a simple task. Keep in mind that CTDIvol and DLP are just approximations of the true patient radiation dose.
In Table 1, a few of the 95% confidence intervals are quite high, for example “joint aspirations/injections”. This is likely due to the procedures being carried out on different body parts on patients of differing body habitus. A subtalar joint injection will have quite a different radiation dose than a sacroiliac joint injection.
At our institution, aside from using CT snapshot mode, there are currently no specific protocols to reduce patient radiation dose for musculoskeletal CT-guided procedures, and practitioners generally use the default CT scanner settings.
ConclusionTop
Our study shows that significant reduction in radiation dose without reduction in procedural accuracy can be achieved by simply lowering the CT scanner voltage and current from their default settings. With careful screening and case selection, in some cases radiation may be avoided all together by utilizing ultrasound or MRI image guidance.
Conflicts of interest
The authors declare no conflicts of interest.
ReferencesTop
[1]Gogna A, Peh WC, Munk PL. Image-guided musculoskeletal biopsy. Radiol Clin North Am. 2008; 46(3):455–473.Article Pubmed
[2]Patel AS, Soares B, Courtier J, Mackenzie JD. Radiation dose reduction in pediatric CT-guided musculoskeletal procedures. Pediatr Radiol. 2013; 43(10):1303–1308.Article Pubmed
[3]Dupuy DE, Rosenberg AE, Punyaratabandhu T, Tan MH, Mankin HJ. Accuracy of CT-guided needle biopsy of musculoskeletal neoplasms. AJR Am J Roentgenol. 1998; 171(3):759–762.Article Pubmed
[4]Huda W. Radiation risks: what is to be done? AJR Am J Roentgenol. 2015; 204(1):124–127.Article
[5]Artner J, Lattig F, Reichel H, Cakir B. Effective radiation dose reduction in computed tomography-guided spinal injections: A prospective, comparative study with technical considerations. Orthop Rev (Pavia). 2012; 4(2):e24.Pubmed
[6]Artner J, Cakir B, Weckbach S, Reichel H, Lattig F. Radiation dose reduction in CT-guided periradicular injections in lumbar spine: Feasibility of a new institutional protocol for improved patient safety. Patient Saf Surg. 2012; 6(1):19.Article Pubmed
[7]Artner J, Cakir B, Reichel H, Lattig F. Radiation dose reduction in CT-guided sacroiliac joint injections to levels of pulsed fluoroscopy: A comparative study with technical considerations. J Pain Res. 2012; 5:265–269.Article Pubmed



