Journal of Radiology and Imaging
An International Peer-Reviewed Open Access Journal
ISSN 2399-8172


- Download PDF
- |
- Download Citation
- |
- Email a Colleague
- |
- Share:
-
- Tweet
-

Journal of Radiology and Imaging
Volume 4, Issue 1, January 2020, Pages 1–6
Rapid communicationOpen Access
Clinical pharmacology, use, and adverse reactions of intravenous iodinated contrast media in computed tomography
-
Brillantino D1,
Ferro T2,
Brillantino C3,
Rossi E3,
Minelli R4,*
 ,
Bignardi E5,
Tufano A6,
Zeccolini R7,and
Zeccolini M8
,
Bignardi E5,
Tufano A6,
Zeccolini R7,and
Zeccolini M8
- 1 University of Campania "Luigi Vanvitelli", Pharmacy and Industrial pharmacy, Caserta, Italy
- 2 Pharmacy Service, District 28 ASL Naples 1 Center, Naples, Italy
- 3 USD Radiology and Ultrasound, PO Pausilipon, AORN Santobono, Pausilipon, Naples, Italy
- 4 Department Life and Health “V. Tiberio”, University of Molise, Via Francesco De Sanctis 1, Campobasso 86100, Italy
- 5 Department of Radiology, Cotugno Hospital, Naples, Italy
- 6 Department of Urology, Sapienza Rome University, Policlinico Umberto I, Rome, Italy
- 7 University of Campania "Luigi Vanvitelli", School of Medicine, Naples, Italy
- 8 UOC of General Radiology, PO Santobono, AORN Santobono-Pausilipon, Naples, Italy
*Corresponding author: Rocco Minelli, M.D., Department Life and Health “V. Tiberio”, University of Molise, Via Francesco De Sanctis 1, Campobasso 86100, Italy. Tel:+393493614286, 0812403198; E-mail: rocco.minelli@libero.it
Received 1 November 2019 Revised 17 December 2019 Accepted 23 December 2019 Published 2 January 2020
DOI: http://dx.doi.org/10.14312/2399-8172.2020-1
Copyright: © 2020 Brillantino D, et al. Published by NobleResearch Publishers. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
AbstractTop
Contrast media are substances used in radiology to improve the visualization of certain body structures subjected to analysis in a medical image. Contrast media are, then, diagnostic drugs because they increase the visibility of organs and tissues and allow the identification of details that otherwise could not be observed. With the introduction of multidetector computed tomography the number of patients undergoing contrast studies has grown exponentially in recent years. In computed tomography the formation of the radiographic image is obtained with the use of contrast media containing iodine atoms, exploiting the different attenuation that the X-ray beam presents in crossing the anatomical districts. The iodinated contrast media are a category of numerous substances formed by even complex molecules that vary considerably in their properties, uses and toxic effects. This article describes the clinical pharmacology, use and adverse reactions of intravenous iodinated contrast media used in computerized tomography, offering all doctors, even non-radiologists, the opportunity for rapid updating.
Keywords: iodinated contrast media; ionic; non-ionic; computed tomography; clinical pharmacology
IntroductionTop
Radiological investigations frequently employ contrast media (CM) which significantly improve the quality of the images, since they detect the anatomical and functional characteristics of an organ and allow us to highlight normal or pathological findings [1]. The formation of the radiographic image exploits the different attenuation that the X-ray beam has in crossing the anatomical districts and this attenuation is in relation with the atomic number (Z) of the substance crossed [1, 2]. Tissues with higher Z will absorb more radiation than tissues with lower Z. The bone, thanks to its high density due to high calcium content, absorbs large amounts of X-rays and appears intensely radiopaque and, therefore, it is easily differentiable from the surrounding tissues. However, in our body there are anatomical regions that have more or less homogeneous densities, similar thickness and chemical composition, so that their discrimination is difficult [1]. CM, when introduced in the body, modify the X-ray absorption of certain structures and, therefore, enhance the differences between the tissues and allow the analysis of details not otherwise evident on the diagnostic images [1, 2]. CM may present a lower or higher radiation absorption than the organs or tissues in which are introduced and they are called "negative" and "positive" respectively. Negative or radiolucent CM are substances in the gaseous state and low density, composed of elements with low Z such as air and carbon dioxide. Substances that contain elements with high Z such as iodine increase the absorption of radiations and are called positive or radiopaque CM [1]. The water-soluble iodinated contrast medium (ICM), commonly delivered through the intravenous route (iv), is required for almost all computed tomography (CT) examinations [1-5]. The ICM allows an optimal evaluation of anatomical structures by increasing the density differences of vessels, organs and tissues, since it determines a strong X-ray absorption in the structures in which it is contained [4-5].
Diagnostic radiologyTop
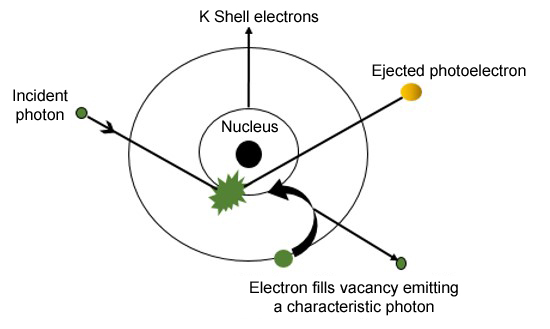
In diagnostic radiology X-rays, that have energies between tens and hundreds of keV, can interact with matter through the photoelectric effect: the photon X strikes an electron of the innermost orbits (generally of the K shell) giving all its energy and the electron acquires a kinetic energy that is equal to the difference between the energy of the incident photon and the bond energy of the electron [2, 6, 7]. It follows the emission of characteristic radiation (with specific wavelength for that type of element), because the gap created in the atom tends to be filled by an electron of an outer orbital with X-ray emission (Figure 1) [6].
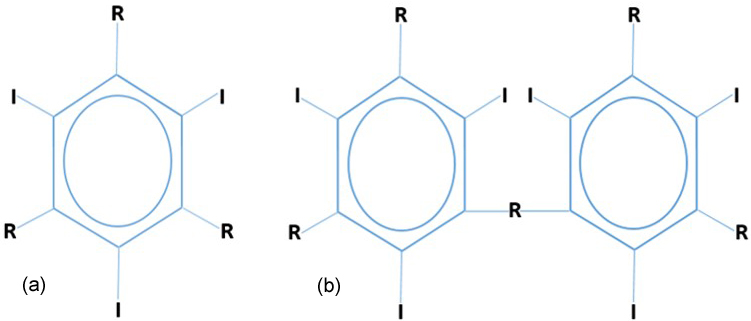
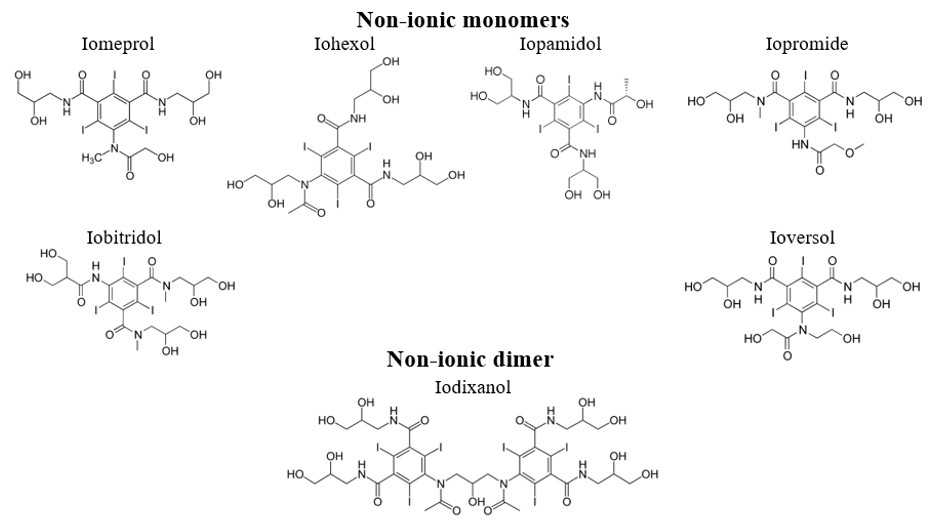
Photoelectric interaction does not occur if the incident photon does not have an energy greater than or equal to the binding energy of inner shell electron. Iodine with its high Z increases the probability of photoelectric absorption since the electron of the shell K has high binding energy of 33.2 keV and presents the maximum X-ray absorption with energy just over 33.2 kVp [2, 5-7]. This is achieved when a relatively low kVp is used and, therefore, for contrast examinations using iodine compounds, optimum technique requires a kVp in the 60-80 range [5, 7]. The attenuation of the X-ray beam increases with the concentration of iodine in the tissue and there is a linear relation between iodine concentration and attenuation. Each milligram of iodine in a milliliter of blood or cubic centimeter of tissue elevates the attenuation by 25 Hounsfield units (HU) [2, 8]. The iodine is, therefore, responsible for the radiopacity of the contrast medium, and the remarkable stability of its bond with benzene, which constitutes the basic structure of the molecule, reduces the risk of the toxic effects from free iodine [1, 3-4, 8, 9]. ICM consists of a benzene ring (monomer) or two benzene rings (dimer) that bind three iodine atoms in positions 2-4-6, while positions 1-3-5 are occupied by the functional groups of the side chains that determine the physicochemical and biological properties of the molecules (Figure 2).
Iodinated contrast mediumTop
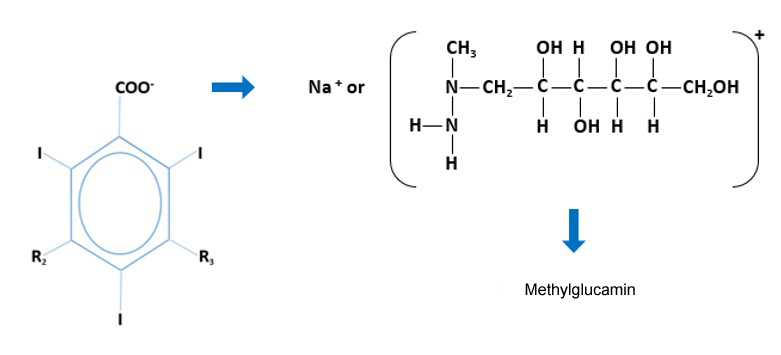
The side chains are made up of carboxyl, amino and hydroxyl groups that influence solubility, osmolality, binding to plasma proteins, tolerability and the route of excretion of ICM. ICMs are divided into ionic and non-ionic [1-4, 8, 9]. Ionic ICMs have the tri-iodinated benzene ring, which has in position 1 a carboxyl group -COOH salified with sodium (Na+) or methylglucamine (Mgl+) [1-4, 8, 9]. The characteristic of these salts is the solubility by electrolytic dissociation in anion and cation and an unfavorable ratio (3:2) between iodine atoms and charged particles (Figure 3) [1, 3, 8]. Therefore, the ionic ICMs are high-osmolar contrast media (HOCMs), having an osmolality about five times higher than that of human plasma (1500–2000 mOsm/kg of H2O compared to 290 mOsm/kg of H2O for plasma) and are currently disused since the charged particles determine a high water recall in the vascular compartment, causing excessive haemodilution, endothelial lesions and nephrotoxicity.
In contrast, non-ionic ICMs do not dissociate in solution since their solubility is guaranteed by hydrophilic side chains and contain three iodine atoms per molecule (ratio 3:1). This involves the reduction of the osmolality (600-900 mOsm/kg H2O) and non-ionic ICMs, called low osmolality contrast media (LOCMs), have greater tolerability and are associated with a lower risk of onset of adverse reactions. Among the non-ionic ICMs, iodixanol is a dimer with six iodine atoms (ratio 6:1) and has an osmolality similar to that of plasma with a lower incidence of undesirable effects than the monomer molecules [1-4, 8-11]. The only ionic ICM with low osmolality is the dimer ioxaglate which in solution produces two ionic particles (ratio 6:2) and has an osmolality similar to non-ionic monomers (Figure 4).
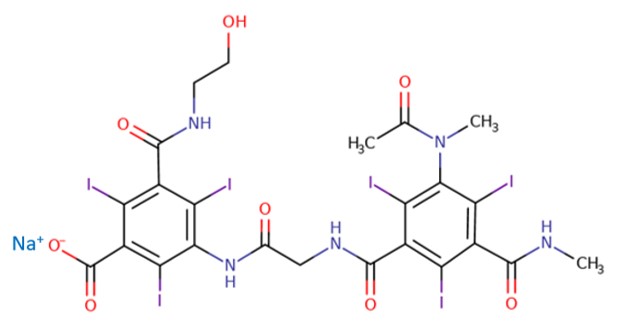
Ioxaglate does not guarantee a low incidence of adverse reactions due to the chemotoxic effects of the electric charges and is mainly used in hemodynamics for its anti-aggregation activity [1-3, 8, 9, 11]. Non-ionic ICMs are characterized not only by the low osmolality and the absence of electric charges, but also by the presence of a greater number of hydrophilic side chains rich in hydroxyls (OH), which increase the solubility of molecules (Figure 5) [1, 2, 8, 11].
Moreover, the more uniform distribution of hydroxyl groups limits the interaction of the lipophilic areas of the molecule (the benzene ring is strongly lipophilic) with plasma proteins and cell membranes and improves the tolerability of contrast [1, 3, 8, 9, 11]. In particular, neurotoxicity has a lower incidence compared to ionic ICMs since non-ionic ICMs are highly hydrophilic molecules, large in size and with low osmolality, so they do not exceed and do not damage the blood-brain barrier [1, 4, 11]. Another fundamental characteristic of the solution of the contrast medium is the iodine concentration, that is the quantity of iodine atoms contained in the unit of volume, expressed in mgI/mL. The higher the concentration of iodine in the contrast, the greater the enhancement obtained due to a more intense photonic attenuation and non-ionic ICMs with iodine concentrations between 300 and 400 mgI/mL are used in CT [1-3, 5, 11, 12]. Finally, an important property of the contrast medium is viscosity, i.e. its ability to flow into the vessels, needles and injection catheters and it is measured in millipascals/sec. A high viscosity hinders the rapid injection of large volumes of contrast, especially in angio-CT studies; moreover, the reduced fluidity of the solution prolongs transit time of the contrast medium in the microcirculation and in the renal tubule with consequent endothelial and renal lesions [1, 4-5, 11, 12]. Viscosity increases with growing molecular size (the dimer iodixanol is more viscous than a non-ionic monomer) and with the increase in iodine concentration and decreases with increasing temperature. Viscosity can be reduced if the preparation is heated to 37°C before iv administration, to allow the rapid injection of contrast and to reduce the risk of extravenous extravasation [1, 2, 4, 5, 8, 9, 11, 12].
DiscussionTop
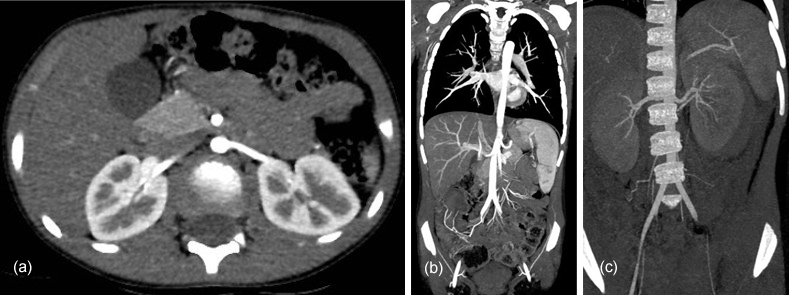
Generally, the antecubital vein of the forearm is the access site of the catheter connected to the automatic injector. The flow rate depends mainly on the caliber of catheter used and 18 or 20 gauge needles allow a high speed of injection. The subsequent administration of physiological solution facilitates progression and compacts the bolus of ICM and reduces the total amount of contrast to be injected [1-5]. The first phase of biodistribution of ICM, called angiography, is characterized by opacification of the veins of the injection site, of the veins of the pulmonary circulation and of the arterial macrocirculation [1, 4, 5, 9, 12]. The arterial enhancement is directly proportional to the speed of injection since a rapid infusion allows that the volume of ICM, which in the unit of time is removed from an artery section due to the push of systolic pressure, to be at once replaced by the next fraction of the same bolus. Furthermore, the arterial enhancement is greater with a high iodine concentration contrast and is, therefore, proportional to IDR (Iodine delivery rate) represented by the product between the flow velocity and the iodine concentration of contrast medium [2, 4, 5, 9, 11, 12]. The later parenchymal arterial phase is characterized by the passage of the ICM from the macrocirculation to the arterial microcirculation which allows the evaluation of organs with significant arterial blood supply, such as the kidney and the pancreas or the visualization of hypervascular parenchymal lesions (Figure 6) [1, 9, 5, 11, 12].
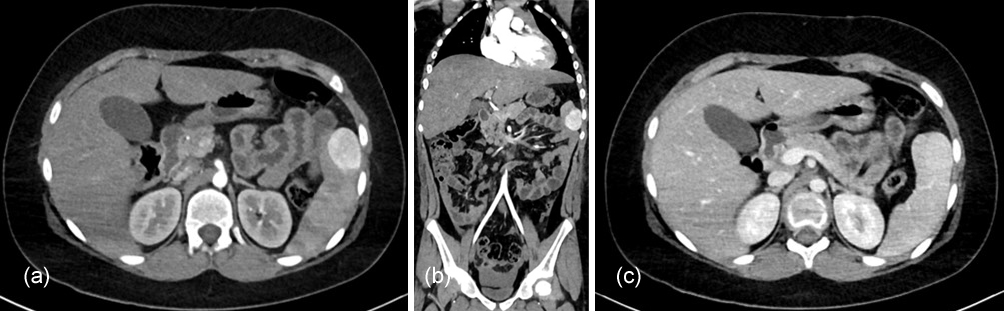
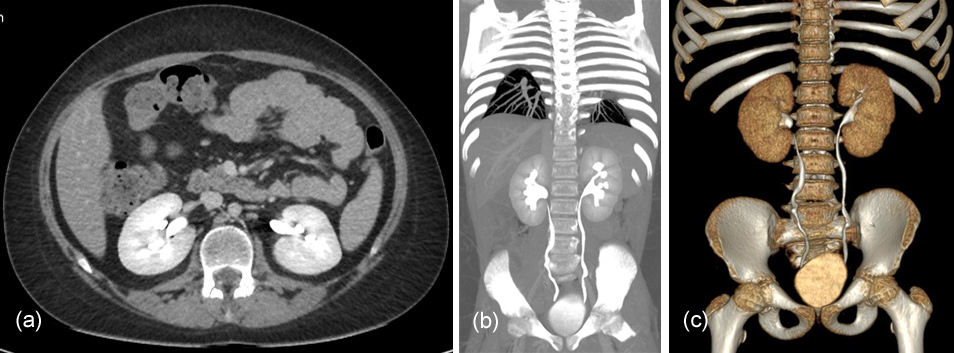
In subsequent venous and late phases, the contrast, due to its high plasma concentration and diffusibility, passes quickly into the interstitial space until it reaches the balance of the concentration between circulating blood and extravascular fluids (Figure 7). The venous and interstitial compartments have a greater volume of distribution than that of the arterial circulation and the enhancement does not depend on the IDR, but on the total quantity of iodine administered, which is the product of iodine concentration and contrast volume injected. Therefore, the CT evaluation of the organs of interest requires the administration of a large volume of ICM rather than its rapid injection and the patient-related factors (e.g., weight, height and age) greatly affect the enhancement [1, 2, 4, 5, 9, 11]. ICM is not metabolized in the body and in the last urographic phase opacifies the urinary tract (Figure 8).
It is eliminated mainly by glomerular filtration without tubular reabsorption and the elimination half-life is approximately two hours in patients with normal renal function [1, 2, 5, 8, 9, 11]. Following iv administration of ICMs, adverse events may occur and more frequently after HOCMs use. Adverse reactions are divided into chemotoxic, anaphylactoid and idiosyncratic [1-3, 9, 13-15]. Chemotoxic reactions are dependent on the dose and plasma concentration of ICM, are potentially predictable and influenced by the osmolality, viscosity and hydrophilicity of the contrast molecule [1, 3, 9, 13, 15]. They are usually mild, spontaneously regress and manifest with nausea, vomiting, altered taste, sensations of heat, sweating, flushing, anxiety, hypotension and bradycardia. Serious, less frequent chemotoxic reactions, are related to the toxic effect on organs and can lead to arrhythmias, pulmonary edema, convulsions and nephrotoxicity.
Kidney is the main target organ, since the ICM is excreted predominantly by glomerular filtration, and contrast-induced nephropathy (CIN) is defined as the impairment of renal function within three days after iv administration of ICM, in absence of other possible causes [1-5, 9, 13-15]. Anaphylactoid reactions are dose-independent, unpredictable and induce the release of histamine and other mediators from mast cells and basophils causing allergic-type manifestations [1, 3, 9, 13-15]. Equally the idiosyncratic reactions are dose-independent and unpredictable, but are characterized by an abnormal and sometimes lethal individual response to the ICM for genetic predisposition [3, 13, 15].
Hypersensitivity reactions
Hypersensitivity reactions are divided according to the time of their onset: in most cases they are immediate and appear within an hour of iv contrast administration; delayed reactions are less frequent and occur between an hour and a week after the injection of ICM [1, 3, 9, 13-15]. Symptoms of the immediate hypersensitivity can be mild, moderate or severe (Table 1). Usually the symptoms are mild and do not require medical treatment, although, in case of need, it is possible to administer antihistamines for urticaria; instead, for moderate symptoms an immediate medical management is essential to avoid the worsening of the patient's clinical condition and for severe, potentially fatal symptoms, the intervention of an anesthesiologist-resuscitator is necessary.
Mild |
Moderate |
Severe |
| Itching | Mild bronchospasm or dyspnea | Malignant arrhythmias |
| Erythema | Diffuse urticaria | Hypotension |
| Urticaria | Persistent vomiting and headache | Severe respiratory distress |
| Cough | Laryngeal and facial edema | State of unconsciousness |
| Rhinorrhoea | Palpitations and abdominal cramps | Convulsions |
| Sneezing | Tachycardia or bradycardia | Progressive angioedema |
| Mild ocular and facial swelling | Hypertension or hypotension | Cardiorespiratory arrest |
ConclusionTop
Finally, late reactions are often mild or moderate, resolve after appropriate treatment and they manifest with urticarial-type skin eruptions, flu-like syndromes and gastrointestinal disorders; severe reactions, such as Steven-Johnson syndrome and toxic epidermal necrolysis are very rare [1, 3, 9, 13-15]. In patients at risk for acute adverse reactions (previous reactions to ICMs, positive history of atopy, asthma and food and drug allergies etc.) pretreatment with corticosteroids, with or without use of antihistamines is a common practice; however, severe reactions can occur despite premedication [9, 14, 15]. The technological advancement with the introduction of ever more performing CT machines and the greater use of the imaging by clinicians, have led to a considerable increase in the number of the examinations carried out with ICM.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, and its late amendments. Additional informed consented was obtained from all patients for which identifying information is not included in this article. Human and animal rights. This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflicts of interest
The authors declare that they have no conflict of interest.
ReferencesTop
[1]Feltrin GP, Zandonà M, Borile V, Rettore C, Miotto D. Fundamentals on iodinated contrast media and adverse reactions. Radiol Med. 2004; 107(4 Suppl 1):8–31.Pubmed
[2]Caschera L, Lazzara A, Piergallini L, Ricci D, Tuscano B, et al. Contrast agents in diagnostic imaging: Present and future. Pharmacol Res. 2016; 110:65–75.Article Pubmed
[3]Singh J, Daftary A. Iodinated contrast media and their adverse reactions.J Nucl Med Technol. 2008; 36(2):69–74.Article Pubmed
[4]Spampinato MV, Abid A, Matheus MG. Current radiographic iodinated contrast agents. Magn Reson Imaging Clin N Am. 2017; 25(4):697–704.Article Pubmed
[5]Bae KT. Intravenous contrast medium administration and scan timing at CT: considerations and approaches. Radiology. 2010; 256(1):32–61.Article Pubmed
[6]Simonetti G. Fisica. In: Simonetti G. Fondamenti di Radiologia Clinica. Napoli: Idelson-Gnocchi Editori.1998. Cap.14, p. 665–666.
[7]Cormode DP, Naha PC, Fayad ZA. Nanoparticle contrast agents for computed tomography: a focus on micelles. Contrast Media Mol Imaging. 2014; 9(1):37–52.Article Pubmed
[8]Shah SN, Sanyal R. Computed Tomography Contrast Media and Principles of Contrast Enhancement. In: Sahani DV, Samir AE. Abdominal Imaging. 2nd ed. Philadelphia, PA: Elsevier; 2017: chap 8, p.60–61.
[9]Pasternak JJ, Williamson EE. Clinical pharmacology, uses, and adverse reactions of iodinated contrast agents: a primer for the non-radiologist. Mayo Clin Proc. 2012; 87(4):390–402.Article Pubmed
[10]Xiao Y, Zeng G, Liu X, Peng C, Lai C, et al. Safety enhancement in adult body computed tomography scanning: comparison of iodixanol versus iohexol. Springerplus. 2016; 5:148.Article Pubmed
[11]Danza FM, Ricci P. I mezzi di contrasto intravascolari organoiodati: caratteristiche fisico-chimiche, indicazioni e contro-indicazioni. In: Gruppo di Lavoro SIRM-SIAARTI-SIN-AINR. Coordinatore Tamburrini O. I mezzi di contrasto in Diagnostica per Immagini. Raccomandazioni all’uso. Reazioni avverse e trattamento. Genova: OMICRON Editrice; 2009; p.66–69.
[12]Faggioni L, Giusti S, Orsi L. I mezzi di contrasto in TC. In: Faggioni L, Paolicchi F, Neri E. Elementi di tomografia computerizzata. Milano: Springer; 2010. Cap.11, p.142–143.Book
[13]Dickinson MC, Kam PC. Intravascular iodinated contrast media and the anaesthetist. Anaesthesia. 2008; 63(6):626–634.Article Pubmed
[14]Bottinor W, Polkampally P, Jovin I. Adverse reactions to iodinated contrast media. Int J Angiol. 2013; 22(3):149–154.Article Pubmed
[15]Beckett KR, Moriarity AK, Langer JM. Safe use of contrast media: what the radiologist needs to know. Radiographics. 2015; 35(6):1738–1750.Article Pubmed


