Journal of Radiology and Imaging
An International Peer-Reviewed Open Access Journal
ISSN 2399-8172


- Download PDF
- |
- Download Citation
- |
- Email a Colleague
- |
- Share:
-
- Tweet
-

Journal of Radiology and Imaging
Volume 8, Issue 1, March 2024, Pages 1–3
Case reportOpen Access
Massive localized lymphedema of the thigh: Pseudosarcoma of the morbidly obese
- 1 Department of Diagnostic Radiology, Dammam Medical Complex, Dammam 754292, Saudi Arabia
*Corresponding author: Dr. Zahra S. M. Husain, Department of Diagnostic Radiology, Dammam Medical Complex, Dammam 754292, Saudi Arabia. E-mail: zahra.4@live.com
Received 3 January 2024 Revised 1 March 2024 Accepted 6 March 2024 Published 12 March 2024
DOI: http://dx.doi.org/10.14312/2399-8172.2024-1
Copyright: © 2024 Husain ZSM, et al. Published by NobleResearch Publishers. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
AbstractTop
Massive localized lymphedema (MLL) is a recently described clinical condition characterized by lymphedema resulting from focally disrupted lymphatic drainage in morbidly obese patients. These patients typically present with long-standing, painless, slow-growing, ill-defined soft tissue masses. The masses are often found in the inner thigh and may resemble liposarcoma both clinically and histologically. Due to its challenging imaging characteristics, MLL poses diagnostic difficulties for clinicians and pathologists. As the global obesity epidemic persists, the incidence of MLL is expected to rise, necessitating awareness and appropriate management strategies. In this context, we present a case of MLL affecting the thigh in a morbidly obese patient. The final diagnosis was given based on patient’s demographics and the presence of lymphedema in other parts of the body.
Keywords: lymphedema; liposarcoma; obesity; sarcoma; computed tomography
IntroductionTop
Morbid obesity is often linked to a constellation of health issues, including hypertension, diabetes mellitus, and various dermatological complications. These skin manifestations encompass conditions such as Acanthosis nigricans, skin tags, leg ulcers, edema, lymphoedema, and plantar hyperkeratosis. Notably, massive localized lymphedema (MLL) emerges as a distinctive disorder primarily affecting individuals with severe obesity. Although the precise epidemiology of MLL remains uncertain, the global surge in obesity rates hints at a potential rise in its prevalence [1]. The term "MLL" was first introduced by Farshid and Weiss in 1998 [2].
MLL is intricately tied to disruptions in lymphatic flow, potentially stemming from the abundance of adipose tissue. Other contributing factors may include prior surgery, injury, or hypothyroidism. Despite these insights, the exact pathogenesis of MLL remains elusive. Consequently, diagnosing MLL poses challenges from clinical, pathological, and radiological perspectives, as the soft tissue lesions associated with MLL can mimic cancerous growths [3].
In some documented cases, MLLs have been surgically excised, often resembling tumors such as liposarcoma or lymphosarcoma upon radiological and histological examination. Consequently, MLL has earned the moniker of a "pseudosarcoma." Furthermore, there is speculation among clinicians that MLL may contribute to the development of angiosarcoma [4].
Case presentationTop
61-year-old male known case of type II diabetes mellitus, essential hypertension and dyslipidemia, presented to the general surgery clinic in Dammam Medical Complex with 10 months history of right thigh swelling. He is morbidly obese with body mass index (BMI) of 58.7. The swelling has increased in size gradually and caused limitations of movement and the patient to seek medical advice for this condition. On examination, there was a very large redundant mass in the superior aspect of the right inner thigh. Both lower limbs were swollen with skin thickening and multiple erythematous papules.
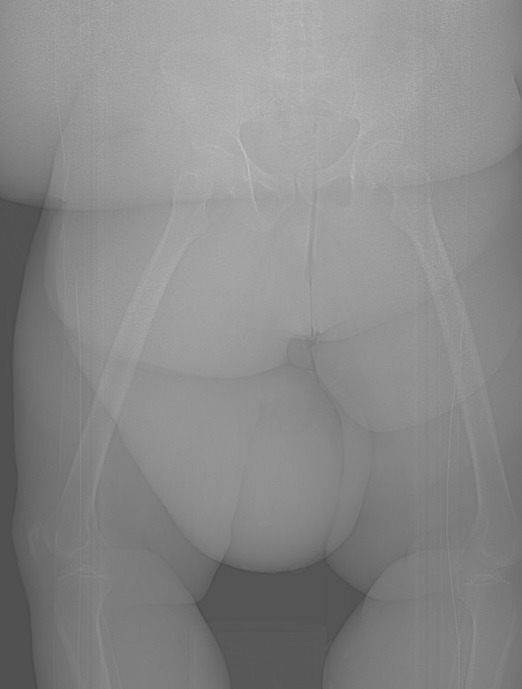
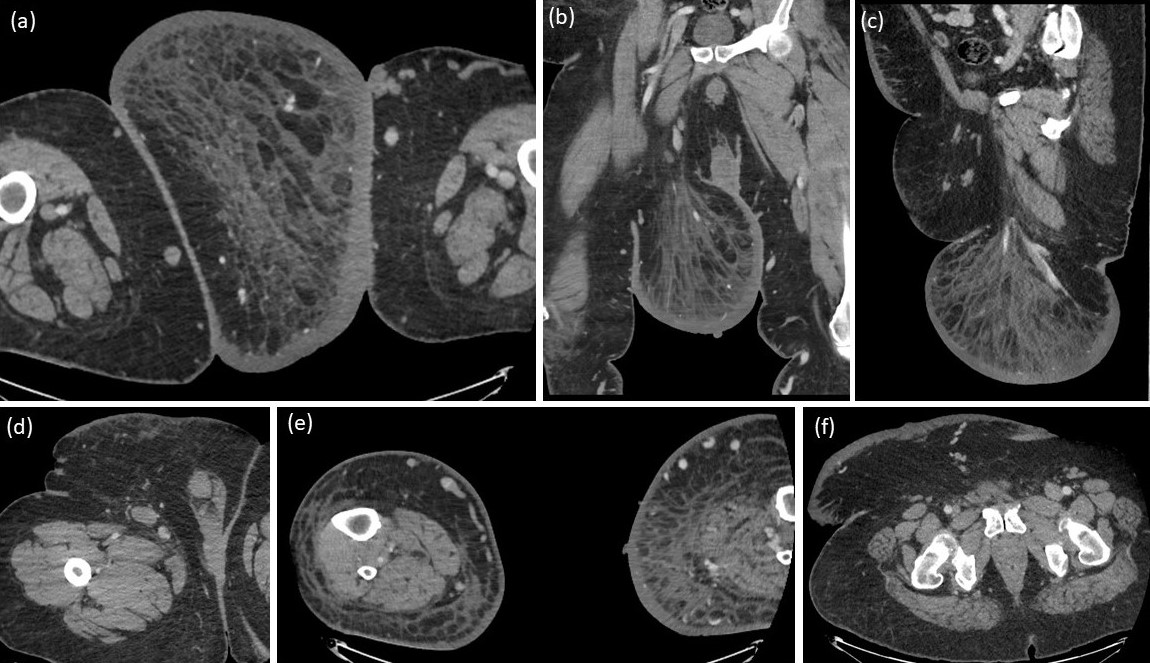
The general surgeon requested enhanced computed tomography (CT) scan (Figure 1 and Figure 2) for the patient as an initial imaging investigation to characterize the nature of the mass. It demonstrated the presence of large mass of fat attenuation in the supero-medial aspect of the right thigh. There is marked skin thickening overlying the mass, involving the anterior abdominal wall as well as bilateral lower thighs. The patient reported history of previous visit to the emergency department two years back with a complaint of left foot pain and swelling. Radiograph was performed at that time (Figure 3) and showed diffuse thickening of the heel-fat pad. Based on the features demonstrated in CT and foot radiograph, the differential diagnosis of massive localized lymphedema (MLL) or atypical lipoma lesion was given.

On follow-up clinic visit, the patient was counseled for the necessity of further imaging with lymphoscintigraphy to confirm the diagnosis of MLL. However, he lost his appointment and preferred to seek a medical advice in his hometown.
DiscussionTop
While direct studies specifically examining the relationship between obesity and the development of lymphedema are lacking, indirect evidence from various sources suggests a connection exists. Animal models also indicate that impaired lymph drainage, stress, and inflammatory disorders play a role in the selective enlargement of adipose tissue associated with lymphoid tissue [5].
In a case series involving 14 patients with morbid obesity, Farshid and Weiss were the first to classify MLL as a distinct, reactive lesion. These investigators observed that MLL shares histological features with well-differentiated liposarcoma (WDL), characterized by mature fat lobules interspersed with expanded connective tissue septa [2]. Although the widened septa resemble the fibrous bands seen in sclerosing WDL, MLL lacks the degree of nuclear atypia present in the latter. All MLL lesions were notably large (33.4 cm and 7408 g), with a nearly 2:1 female-to-male predominance [2].
Recent studies emphasize that this pseudosarcomatous, tumefactive benign entity primarily affects the obese population, with a female bias. The lesions vary in size, ranging from 19.5 to 61.5 cm. However, there remains controversy in the literature regarding the association of pain with MLL [6]. Clinically and histologically, distinguishing MLL from other tumor-like processes (such as lipoma, lipomatosis, WDL, desmoid-type fibromatosis, angiomatosis, lymphangiomatosis, angiomyoma, angiosarcoma, low-grade fibroblastic neoplasm, and myxoidliposarcoma) can be challenging unless one is familiar with this condition. Notably, a history of morbid obesity and prominent skin changes, including induration and "peaud'orange" appearance due to congested dermal lymphatics, aids in accurate diagnosis [5].
While there is a preference for the inner thigh, other anatomical sites—such as the lower abdominal wall, suprapubic region, mons pubis, vulva, inguinoscrotal area, penis, perianal region, popliteal fossa, lower leg, and arm—have also been documented. The pathogenesis remains uncertain, with potential associations including lymphatic obstruction related to extensive adipose tissue, trauma, surgical interventions, and/or hypothyroidism. The lymphatic system functions by following vessels, facilitating the return of extravasated fluids and molecules to the circulatory system. Dysfunction in this system can lead to fluid accumulation, resulting in lymphedema [7, 8].
Histologically, sectioning of the mass reveals abundant mature adipose tissue interspersed with thick, edematous fibrous septae and substantial edema. In some instances, dystrophic calcification may be present [4]. Recent reports describe additional features, including dermal fibrosis, expansion of fibrous septa between fat lobules with increased stromal fibroblasts, lymphatic proliferation, lymphangiectasia, multinucleated fibroblastic cells, and marked vascular proliferation [1].
Radiologically, the CT and MRI appearance of the lesion resembles a large pendulous mass of adipose tissue, devoid of fascial or muscle involvement. This directly correlates with the histopathological findings of dermal fibrosis, edema, and fat partitioned by fibrous septae. Specifically, edema tracks along the fibrous septa in a lace-like pattern, accompanied by associated dermal thickening. Contrast administration reveals only mild enhancement in the dermis, consistent with the features observed in lymphedema [9-11].
In the context of treating MLL, surgical intervention stands as the gold standard. Its objectives include restoring mobility particularly for large lesions in the inner thigh that may hinder ambulation, preventing recurrent infections arising from mechanical dermal abrasion, and confirming the diagnosis. Conservative approaches, such as antibiotic therapy for associated cellulitis and the use of compression dressings alone, have demonstrated limited success. Given that MLL's underlying cause is linked to lymphatic obstruction, persistence or recurrence of the lesion is anticipated even after surgical resection [12, 13].
While MLL is generally considered benign, it is essential not to underestimate its significance. Left untreated, MLL can undergo transformation into more aggressive conditions, such as angiosarcoma or Stewart-Treves syndrome [3]. This cautionary note is particularly relevant in cases where patients decline surgical intervention, as exemplified in our current scenario. Furthermore, there have been documented instances of squamous cell carcinoma and cutaneous angiosarcoma arising from long-standing MLL [5].
While we lack the final histopathological diagnosis in our case, the constellation of patient’s demographics, clinical presentation along with the radiological features supports the diagnosis of MLL.
ConclusionTop
While our comprehension of MLL has expanded since its initial identification, diagnostic complexities persist due to its resemblance to malignant conditions. The case presented here serve as archetypal example of the typical MLL demographic. As global obesity rates continue to rise, a comprehensive understanding of MLL becomes increasingly crucial. Recognizing this distinct entity, along with clinical and gross pathological correlations, plays a pivotal role in distinguishing MLL from its various morphological mimics. Future research endeavors should prioritize elucidating its pathophysiology, assessing nonsurgical interventions, and investigating potential associations with comorbidities, including angiosarcoma.
Conflicts of interest
Authors declare no conflict of interest.
ReferencesTop
[1]Khanna M, Naraghi AM, Salonen D, Bhumbra R, Dickson BC, et al. Massive localised lymphoedema: Clinical presentation and MR imaging characteristics. Skeletal Radiol. 2011; 40(5):647e52.Article Pubmed
[2]Farshid G, Weiss SW. Massive localized lymphedema in the morbidly obese: A histologically distinct reactive lesion simulating liposarcoma. Am J Surg Pathol. 1998; 22(10):1277–1283.Article Pubmed
[3]Kotidis E, Cepaityte D, Petrakis G, Sapalidis K, Kanellos I. Massive localized lymphedema in the morbidly obese patient: a clinical entity mimicking lymphosarcoma. Wounds. 2015, 27(9):249–252.Article Pubmed
[4]Porrino J, Walsh J. Massive localized lymphedema of the thigh mimicking liposarcoma. Radiol Case Rep. 2016, 11(4):391–397.Article Pubmed
[5]Manduch M, Oliveira AM, Nascimento AG, Folpe AL. Massive localisedlymphoedema: a clinicopathological study of 22 cases and review of the literature. J Clin Pathol. 2009; 62(9):808–811.Article Pubmed
[6]Jabbar F, Hammoudeh ZS, Bachusz R, Ledgerwood AM, Lucas CE. The diagnostic and surgical challenges of massive localized lymphedema. Am J Surg. 2015; 209(3):584–587.Article Pubmed
[7]Bahrami A, Ronaghan JE, O-Yurvati AH. Pseudosarcoma of the thigh: a rare case of massive localized lymphedema. Int Surg. 2015; 100(3):461–465.Article Pubmed
[8]Wu D, Gibbs J, Corral D, Intengan M, Brooks JJ. Massive localized lymphedema: additional locations and association with hypothyroidism. Hum Pathol. 2000; 31(9):1162–1168.Article Pubmed
[9]Goshtasby P, Dawson J, Agarwal N. Pseudosarcoma: massive localized lymphedema of the morbidly obese. Obes Surg. 2006; 16(1):88–93.Article Pubmed
[10]Moon Y, Pyon JK. A rare case of massive localized lymphedema in a morbidly obese patient. Arch Plast Surg. 2016; 43(1):125–127.Article Pubmed
[11]Lobato RC, Zatz RF, Cintra Junior W, Modolin ML, Chi A, et al. Surgical treatment of a penoscrotal massive localized lymphedema: case report. Int J Surg Case Rep. 2019; 59:84–89.Article Pubmed
[12]Ba-Shammakh SA, Haj-Freej HM, Al-Naggar YS, et al. Massive Localized Lymphedema: Two Case Studies and Diagnostic Challenges. Cureus. 2023; 15(10):e47092.Article Pubmed
[13]Baydar DE. Massive localized lymphedema in an unreported location (Retroperitoneum). Diagn Pathol. 2018; 13:89.Article Pubmed



