Journal of Traumatology and Clinical Orthopaedics
An International Peer-Reviewed Open Access Journal
ISSN 2399-8180


- Download PDF
- |
- Download Citation
- |
- Email a Colleague
- |
- Share:
-
- Tweet
-

Journal of Traumatology and Clinical Orthopaedics
Volume 2, Issue 1, October 2020, Pages 1–6
Original researchOpen Access
Premature discontinuation of a randomized comparison between a new implant Dynaloc® and cancellous screws for femoral neck fractures: An ethical dilemma
- 1 Department of Orthopaedics, Aarhus University Hospital, Aarhus, Denmark
- 2 Department of Orthopaedics, Randers Regional Hospital, Randers, Denmark
*Corresponding author: Lars C. Borris, Department of Orthopaedics, Aarhus University Hospital, Palle-Juul Jensens Boulevard 99, DK 8200 Aarhus N, Denmark. Tel.: +45 51481740; E-mail: larbor@rm.dk
Received 4 August 2020 Revised 15 September 2020 Accepted 21 September 2020 Published 1 October 2020
DOI: http://dx.doi.org/10.14312/2399-8180.2020-1
Copyright: © 2020 Borris LC, et al. Published by NobleResearch Publishers. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
AbstractTop
Background and purpose: To evaluate the clinical efficacy of Dynaloc®, a new implant for fixation of femoral neck fractures, which comprises 3 cancellous screws fixed in a small side plate. Patients and methods: Patients older than 50 years with fresh femoral neck fractures were randomly allocated to osteosynthesis with Dynaloc® or cancellous screws. The primary endpoint was leg length discrepancy due to femoral neck shortening. The secondary endpoints were WOMAC, EQ-5D, and Harris hip scores after 12 months as well as the fracture healing properties, all reoperations, and adverse events after 24 months. Results: Mean patient age was 71.9 (SD 11.8) years; 60% were women. Fracture types were mainly Garden I and II. No significant differences in the primary or secondary endpoints between the Dynaloc® and cancellous screw groups were observed. Seventeen patients experienced at least one reoperation: in the Dynaloc group 2 patients had THA and 5 had the implant removed additionally one patient developed infection requiring operation, in the screw group 4 had an arthroplasty (1 HA and 3 THA) and the implants were removed in 5. Avascular necrosis of the femoral head was verified in three patients in the Dynaloc® group. Conclusion: A firm conclusion cannot be drawn from this study because of small numbers, but we found no differences in terms of limb length and other outcome measures between the groups at one year, which cannot justify the use of Dynaloc® due to the frequent complications related to the implant.
Keywords: hip fracture; cancellous screws; Dynaloc®; implant removal
IntroductionTop
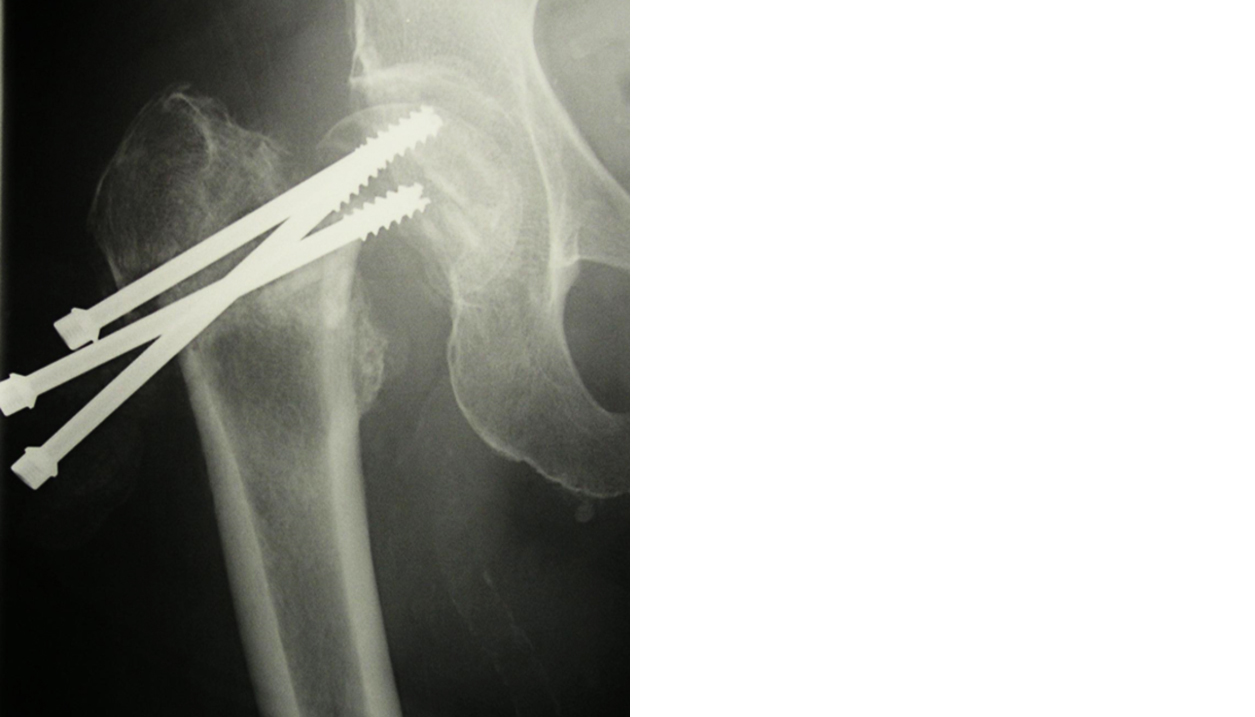
Femoral neck fractures (FNFs) are common in the elderly and comprise ~50% of all fractures around the hip. In Denmark the most commonly used methods of internal fixation are osteosynthesis with multiple cancellous screws (i.e., ≥2) or dynamic hip screw (DHS). Internal fixation of FNFs had a high reoperation rate, up to 27 % in patients between 55 and 70 years of age in a Scandinavian register study, compared with other treatment forms such as hemi- or total hip arthroplasty (HA or THA) [1]. Failure after screw fixation is mostly caused by individual screw backout due to rotational forces resulting in shortening of the femoral neck and subsequent leg shortening. In severe cases, even loss of fixation and fracture collapse can be seen (Figure 1). In a retrospective follow up study of healed FNFs leg length discrepancy (LLD) due to femoral neck shortening was seen in >60%, resulting in significantly lower ratings of physical functioning (SF 36) and quality of life (EQ-5D) [2].
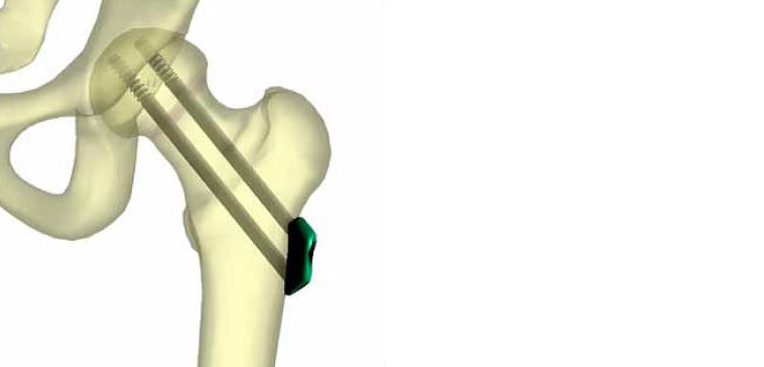
Dynaloc® is a new fixation device for treating FNFs; it comprises three screws locked at a fixed angle in a small side plate, which itself is not fixed to the femur (Figure 2). Stability testing of the same plate with three Hansson pins called the Hansson Pinloc® system compared with two or three pins alone in a proximal femur fracture model has been performed to calculate torsional stiffness, torque at failure and failure energy. The new implant significantly improved all parameters [3]. Comparable results have been obtained with similar testing of the Dynaloc® implant.
This study hypothesized that fracture fixation with Dynaloc® could reduce leg shortening because of a more rigid fracture fixation resulting in less collapse at the fracture site compared with three cancellous screws.
Materials and methodsTop
This randomized, comparative, controlled study between Dynaloc® and cancellous screws was performed at our hospital. Patients admitted to the hospital following a low-energy trauma to the hip with FNF AO/OTA types 31-B1 [4] were enrolled. We used the first-generation Dynaloc® implant (Swemac AB, Lindköping, Sweden), made of a titanium alloy, consisting of three cannulated screws (6.7 mm in diameter) locked in a small plate. The plate was in three sizes 6, 9, and 12 mm. A specific surgical technique was used to insert the implant. The plate size was decided using X-ray in anteroposterior and axial projections, and then 3 guide wires were placed through the femoral neck and head in an inverted triangle configuration [5, 6] using a special drill guide. The screw lengths were measured and finally, after predrilling over the guide wires, the screws were fixed in the subchondral bone to obtain compression at the fracture site and locked in the plate using locking nuts. To gain experience with the new equipment before starting the study, two surgeons operated a preliminary cohort of 10 patients (mean age 77.4 (61–90) years) with fresh FNFs; the patients were followed up radiologically after 3–4 months. The two surgeons who performed the preliminary series served as supervisors in this study.
The cancellous screws used in the screw group were cannulated screws (7 mm) made of steel and placed in an inverted triangle configuration using a standard technique.
Patients were randomly assigned to operative treatment with Dynaloc® or three cancellous screws using a centralized 24-h computerized, randomization system, which allowed immediate randomization via the internet. All included patients provided written informed consent after having received oral and written information on all study procedures, including the benefits and risks, before randomization. The primary outcome measure was LLD within 3 postoperative months, and the secondary outcome measures included a measure of function and pain (WOMAC) and a generic utility measure (EQ-5D) at inclusion and 1 year after inclusion. In addition, Harris hip score was assessed after one year. During the study clinical and radiographic healing rates and all complications, such as mortality, femoral shaft fracture, femoral head necrosis, non-union, malunion, implant breakage or failure, infection, and any reoperation related to the hip in question were noted with 2 years' follow-up. Adverse events throughout the study were reported within 24 h after the investigator noted an event. Serious adverse events (SAEs) were death; a life-threatening experience; initial or prolonged inpatient hospitalization; persistent or significant disability/ incapacity, resulting in permanent damage to the body structure and needing medical or surgical intervention; and incidents considered significant by the investigator for any other reason.
Table 1 shows the inclusion and exclusion criteria used in this study. After inclusion, data on age, sex, weight, height, body mass index, and smoking habits were obtained. All fractures were classified using the Garden classification [7]. Patients also filled out questionnaires on WOMAC, and EQ-5D regarding their status 14 days before the fracture. The operative procedure was performed as soon as possible after randomization; time to operation and operation duration were recorded routinely. Patients were placed on a traction fracture table, and the fracture was reduced with traction and internal rotation of the leg using fluoroscopic control with a C-arm. Screw insertion was performed using a percutaneous technique in both groups. Screw placement was documented postoperatively by downloading the fluoroscopic images in two planes (anteroposterior and lateral) in the central electronic picture archiving and communication system of the hospital. All patients received a preoperative antibiotic, i.e., dicloxacillin or cefuroxime (single dose), and a postoperative antithrombotic prophylaxis using dalteparin (Fragmin; 5,000 IU, administered subcutaneously once daily). Immediate weight bearing was allowed in both groups.
| Inclusion criteria |
| Men or women with a subcapital femoral neck fracture (stable or unstable) confirmed with anteroposterior and lateral hip radiographs, computed tomography, or magnetic resonance imaging |
| Patients between 50 and 69 years of age with any Garden type femoral neck fracture |
| Patients >70 years of age with a femoral neck fracture Garden type I or II |
| Patients >70 years of age with a femoral neck fracture Garden type III or IV and contraindication to hip arthroplasty |
| Operative treatment within 4 days (i.e., 72 h) of presenting to the hospital |
| Patient was ambulatory prior to fracture, although they may have used an aid such as a cane or a walker |
| Anticipated medical optimization of the patient for operative fixation of the fracture |
| Provision of informed consent by patient |
| Low energy fracture (defined as a fall from a standing height) |
| No other major trauma |
| Exclusion criteria |
| Retained implant around the affected hip |
| Abnormal opposite hip, making endpoint evaluation impossible |
| Infection around the hip (in the soft tissue or bone) |
| Patients with disorders of bone metabolism other than osteoporosis (e.g., Paget's disease or renal osteodystrophy) |
| Moderate or severe cognitive impairment |
| Patients with Parkinson's disease (or dementia or other neurological deficit) that is severe enough to compromise rehabilitation |
| Possibleproblems with maintaining follow-up, based on the investigator's assessment |
After discharge, patients were followed up after 3 months, 1 year, and 2 years. At first visit, the patient was examined clinically and a radiograph of the hip with anteroposterior and lateral projections was performed to assess fracture healing. Blinded measurement of LLD between the operated and non-operated leg was conducted by a physiotherapist. For blinding the scar on the operated side was hidden with a strip of tape and a similar strip of tape was placed on the non-operated side and patients were instructed not to reveal the side of the fracture to the examiner. LLD was measured using two methods. A direct method by tape measure was performed from the anterior superior iliac spine to the medial malleolus, with the patient in the supine position. In addition, an indirect measuring method was performed using a combination of wooden blocks with heights of 5, 10, and 20 mm, applied under the short leg with the patient in the standing position, to correct the pelvic tilt. LLD was graded as no shortening (0 mm), mild shortening (<5 mm), moderate shortening (5–10 mm), and severe shortening (>10 mm). At the 12-month follow up WOMAC, and EQ-5D were reassessed; the patients completed self-administered questionnaires. Moreover, clinical examination and functional status evaluation based on Harris hip score were performed. The 24-month follow up was conducted via telephone to document whether any revision surgery of the hip had already been performed or planned.
Sample size calculation was based on a previous long-term follow up study, which reported a 66% rate of objectively measured femoral neck shortening on radiographs following FNF treated with osteosynthesis with cancellous screws [3]. Thus, our sample size was based on pairwise comparisons of Dynaloc® vs. cancellous screws for the primary outcome (leg shortening). All statistical hypotheses were two-sided. We chose an alpha level of 0.05 for the primary outcome (any leg shortening) and a beta level (power) of 0.80. Furthermore, we defined a clinically relevant reduction of leg shortening by 50% (i.e., from 66 to 33%). The calculation resulted in a sample size of 75 patients in each group, considering a dropout rate of at least 10% during the study. To include an adequate number of younger patients, randomization was weighted 2:1 according to age, i.e., below and above 70 years. Thus, in each group, 50 patients aged <70 years and 25 patients aged >70 years should be included. All outcome analyses were performed on an intention to treat principle. The effect of the two treatments on the primary outcome measure, LLD, was statistically estimated with the following covariates: (1) age (i.e., 50–69 years or >70 years), (2) Garden fracture type, and (3) no shortening vs. any shortening.
We used independent t-test and Wilcoxon (Mann-Whitney) rank-sum test to compare continuous outcomes between groups and Fisher exact and Chi-Square tests were used to compare categorical outcomes. All statistical analyses were performed using Stata version 15.1.
The study was approved by the Regional Ethics Committee (No 40904), and the Danish Data Protection Agency was notified. It was registered at ClinicalTrials.gov (NTC 02030431).
ResultsTop
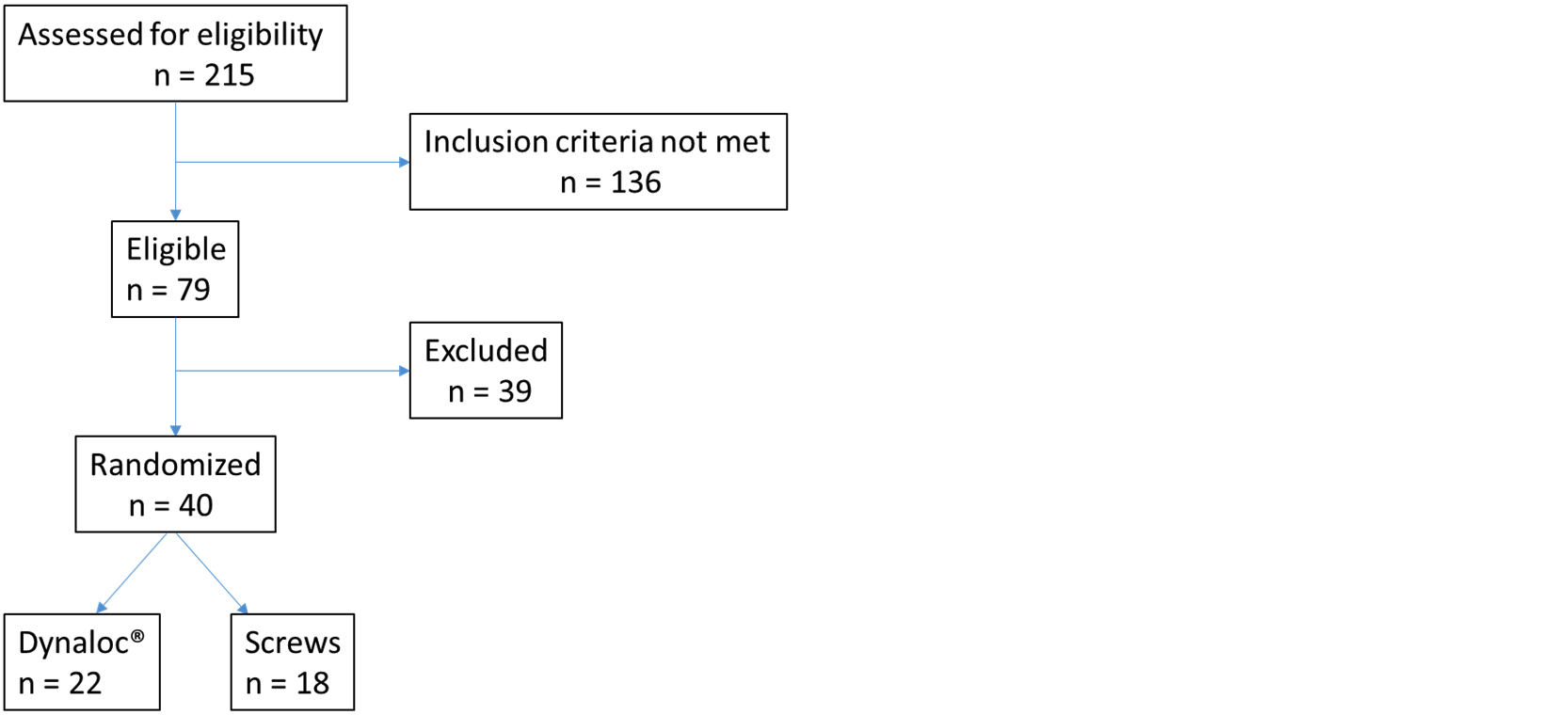
The study was initiated March 2014 and after approximately 18 months 5 patients in the Dynaloc® group vs. only one in the screw group had the implant removed due to local discomfort. At the same time a redesign of the implant was launched in order to obtain a better patient acceptance. On this basis, we decided to prematurely stop the study after inclusion of a total of 40 patients because we felt that a continuation of the study would be unethical, 22 patients were allocated to treatment with Dynaloc® and 18 to treatment with cannulated screws. A Consolidated Standard of Reporting Trials (CONSORT) flow diagram describing the patient household in the study is shown in Figure 3. Patient demographics, including the Garden fracture type, time from admission to surgery, and duration of operation are listed in Table 2. The groups were comparable in demographic variables. The majority of fractures were undislocated (Garden fracture types I and II). The time from hospital admission to surgery was comparable between groups. Thirteen different surgeons performed the Dynaloc® operations and 12 operated with screws and there was a great deal of overlap, so most surgeons operated in both groups. Closed reduction was successful in all cases. The duration of operation was significantly longer in the Dynaloc® group than in the screw group (p < 0.05) (Table 2).
| Dynaloc® group N=22 |
Screw group N=18 |
||
| Sex (M/F) | 10/12 | 6/12 | |
| Age, years* | 73 (13.5) | 70.6 (9.4) | |
| <70 years | 11 | 10 | |
| >70 years | 11 | 8 | |
| Weight, kg* | 71 (16.4) | 68.6 (13.5) | |
| Height, cm* | 172.1 (11.2) | 173.6 (8.8) | |
| BMI, kg/m2* | 23.7 (3.9) | 22.6 (3.1) | |
| Smoker | |||
| Yes | 5 | 5 | |
| No | 17 | 6 | |
| Previous | 0 | 6 | |
| No information | 0 | 1 | |
| Garden fracture stage | |||
| I | 9 | 6 | |
| II | 11 | 5 | |
| III | 1 | 4 | |
| IV | 1 | 3 | |
| Side (right/left) | 10/12 | 9/9 | |
| Time from admission to surgery, h* | 15.2 (8.9) | 16.9 (10.4) | |
| Duration of operation, min** | 51.9 (11.5) | 43.9 (19.3) | |
Values are mean (SD). BMI: body mass index; *Not significant; **p<0.05
During the follow up visit at 3 months, 21 patients in the Dynaloc® group and 13 in the screw group were examined. Table 3 shows the results of the blinded leg length measurements and the radiological outcomes. No shortening was noted in 12 patients in the Dynaloc® and in 6 patients in the screw group. Various degrees of LLD were noted in the rest. Clinical and radiological healing was observed in all cases. Radiographs showed uncomplicated fracture healing in 15 patients in the Dynaloc® and in 10 patients in the screw group. Femoral neck shortening was noted in the remaining patients. No statistically significant differences were observed between the groups in terms of LLD or healing. The relationship between radiological femoral neck shortening and measured LLD was not consistent (Table 3).
| LLD | 0 mm |
Mild <5 mm |
Moderate 5-10 mm |
Severe >10 mm |
Total |
| Dynaloc® group (N=21)a | |||||
| Uncomplicated healing | 8 |
1 |
6 |
0 |
15 |
| Femoral neck shortening | 4 |
0 |
1 |
1 |
6 |
| Screw group (N=13)b | |||||
| Uncomplicated healing | 5 |
0 |
5 |
0 |
10 |
| Femoral neck shortening | 1 |
0 |
1 |
1 |
3 |
| Total | 18 |
1 |
13 |
2 |
34 |
LLD: leg length discrepancy; aOne patient missing; bFive patients missing.
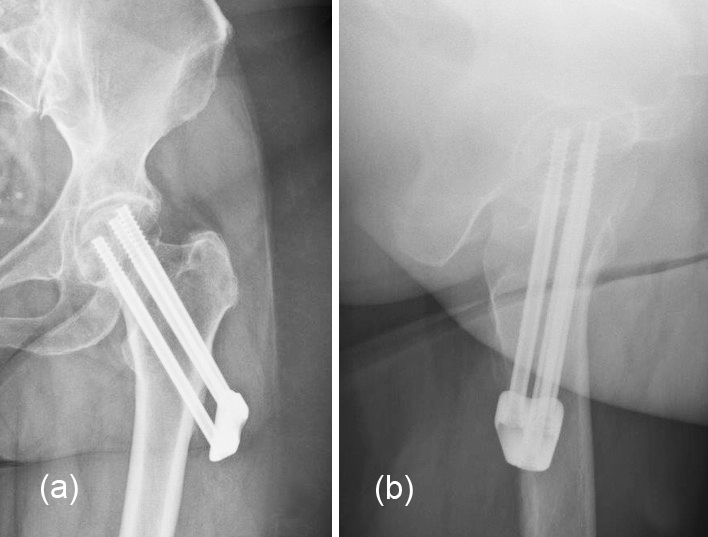
During the follow up at one year, 17 patients in the Dynaloc® group and 15 patients in the screw group answered the WOMAC, and EQ-5D questionnaires. No statistical differences between the groups in any of the scores were found. The mean (SD) Harris hip score after one year was 86.1 (3.0) in the Dynaloc® group and 81 (4.7) in the screw group (p0.4). Tables 4a and 4b show the results of the 2-year follow up, including the time to reoperation of the individual patients in each group. No statistically significant difference between the groups in the mean (SD) time to reoperation [Dynaloc® group, 336.8 (119.4) days; screw group, 336.2 (166.1) days (p=0.7)] was noted. Seventeen patients had at least one reoperation (eight in the Dynaloc® group and nine in the screw group). Two patients in the Dynaloc® group had total hip arthroplasty (THA), one had an isolated screw penetration, the other developed AVN diagnosed on a computed tomography (CT) scan. Additionally, two patients in the Dynaloc® group developed AVN of the femoral head in the later part of the 2-year study period, confirmed on radiographs in one and magnetic resonance imaging (MRI) in the other, and underwent THA after study completion. In the screw group, four patients had arthroplasty due to fracture collapse. Six and five patients in the Dynaloc® and screw group, respectively, had implant removal. Figure 3 illustrates the span of protrusion into the soft tissues observed in one of the Dynaloc® patients who had the implant removed. An SAE was observed in six cases (five in the Dynaloc® group and one in the screw group; Tables 4a and 4b). Two patients in the Dynaloc® group and one in the screw group died of causes unrelated to the hip fracture.
Case no. |
Sex |
Age |
Event type |
Event description |
Days to event |
7073 |
M |
53 |
SAE |
Intrapelvic hematoma |
2 |
7077 |
F |
66 |
Reoperation |
THA |
42 |
7069 |
M |
57 |
Reoperation/SAE |
Wound infection |
66 |
6783 |
M |
79 |
SAE |
Death |
200 |
7073 |
M |
53 |
Reoperation |
Implant removal |
287 |
6771 |
F |
78 |
Reoperation |
Implant removal |
327 |
6772 |
M |
89 |
SAE |
DVT |
328 |
7071 |
F |
60 |
Reoperation |
Implant removal |
371 |
7063 |
F |
63 |
Reoperation |
Implant removal |
389 |
6770 |
F |
85 |
Reoperation |
Implant removal |
413 |
7083 |
M |
51 |
Reoperation |
Implant removal |
433 |
7073 |
M |
53 |
Reoperation |
THA |
625 |
6781 |
F |
91 |
SAE |
Death |
657 |
SAE: serious adverse events; THA: total hip arthroplasty; aTwo patients who developed avascular necrosis had a THA after completion of the study.
Case no. |
Sex |
Age |
Event type |
Event description |
Days to event |
7064 |
F |
61 |
Reoperation |
HA |
54 |
7062 |
M |
67 |
Reoperation |
THA |
76 |
6774 |
F |
86 |
SAE |
Death |
145 |
7074 |
F |
63 |
Reoperation |
THA |
307 |
7076 |
F |
54 |
Reoperation |
Implant removal |
358 |
6780 |
F |
82 |
Reoperation |
Implant removal |
374 |
7072 |
F |
59 |
Reoperation |
Implant removal |
412 |
7082 |
M |
69 |
Reoperation |
Implant removal |
464 |
7068 |
M |
67 |
Reoperation |
THA |
470 |
7080 |
M |
91 |
Reoperation |
Implant removal |
511 |
SAE: serious adverse events; HA: hemiarthroplasty; THA: total hip arthroplasty.
DiscussionTop
To the best of our knowledge, this is the first randomized comparison between the first generation Dynaloc® and screw osteosynthesis in patients with fresh FNF. Since May this year (2020) a new European Union regulation (EU) 2017/745 has been put into force [8] according to which clinical testing will be needed of all new devices before marketing. We find it of great importance because only direct comparisons in a real clinical setting can show the advantage and the disadvantages of a new implant. In our case, continuation of the study would have been unethical when considering that the new implant rather early in the investigation showed a lower patient acceptance compared to screws and that the new design of the implant would potentially be better tolerated. In 2019, after we had stopped our study, a preliminary report was published on a randomized comparison between Hansson Pinloc®, Dynaloc´s sister-implant, and Hansson pins alone in 439 FNF patients which showed no difference in terms of fixation failures and reoperations in the two groups followed up after one year [9] very similar to our findings after two years.
Thus, despite the biomechanical advantage in the laboratory of Hansson pins or cannulated screws locked in a plate over pins and screws alone [3] the clinical outcomes were not so advantageous.
The rationale behind the concept is that when the pins or screws are locked in a plate the risk of individual screw backout is overcome because the construct acts like one unit, which should reduce the risk of fracture collapse because it could better withstand rotational forces [3]. The plate, which was used in our study was sized so that the thickness was almost the same as the hip screw plate. This may have caused the patient discomfort because it was rather prominent and could be felt under the skin and when the patients lay on the operated side and were sitting and cycling, which was accentuated if the implant backed out as shown in Figure 4. In the redesign of the implant the plate thickness has been much reduced and at the same time the angle between the screws and the plate is reduced from 130 degrees to 120 and 125 degrees to move the plate up on the femur to be sheltered by the greater trochanter. In our opinion, no implant could overcome the tendency of shortening of the femoral neck at the fracture site because the natural healing processes remove dead bone that has lost blood supply at the time of the accident accentuated by high age, osteopenia or osteoporosis.
It could be argued that the plate should be fixed to the femur in order to avoid protrusion of the material into the soft tissues necessitating implant removal. However, locking the screws in the plate could inhibit the dynamic fracture compression. This has already been reported on another system with locking screws and the plate fixed to the femur, which resulted in more than 50% screw breakage or screw penetration of the femoral head [10].
Many surgeons prefer to use DHS for osteosynthesis of FNFs to obtain a more reliable fixation. However, a recent large multinational, multicenter, randomized study comparing osteosynthesis of FNFs with screws and osteosynthesis with DHS, irrespectively of Garden type and patient age, no statistical differences were reported between the two surgical modalities in terms of healing or complications, however, there was a higher absolute number of fracture collapse in the screw group and more avascular necrosis (AVN) of the femoral head in the DHS group [11].
ConclusionTop
Firm conclusions are difficult due to low numbers, however, we did not find any differences in terms of limb length and measured outcomes between the groups at one year which could not justify to use the tested implant due to the observed discomfort reported by the patients.
Funding
The online randomization system used was funded by Swemac AB, Lindköping, Sweden.
Conflicts of interest
Authors declare no conflict of interest.
ReferencesTop
[1]Bartels S, Gjertsen JE, Frihagen F, Rogmark C, Utvåg SE. High failure rate after internal fixation and beneficial outcome after arthroplasty in treatment of displaced femoral neck fractures in patients between 55 and 70 years. Acta Orthop. 2018; 89(1):53–58.Article Pubmed
[2]Zlowodzki M, Brink O, Switzer J, Wingerter S, Woodall J, et al. The effect of shortening and varus collapse of the femoral neck on function after fixation of intracapsular fracture of the hip: a multi-centre cohort study. J Bone Joint Surg Br. 2008; 90(11):1487–1494.Article Pubmed
[3]Brattgjerd JE, Loferer M, Niratisairak S, Steen H, Strømsøe K. Increased torsional stability by a novel femoral neck locking plate. The role of plate design and pin configuration in a synthetic bone block model. Clin Biomech 2018; 55:28–35.Article Pubmed
[4]Fracture and dislocation compendium. Orthopaedic Trauma Association Committee for coding and classification. J Orthop Trauma. 1996; 10(Suppl 1:v-ix):1–154.Pubmed
[5]Yang J-J, Lin L-C, Chao C-H, Chuang S-Y, Wu C-C, et al. Risk factors for nonunion in patients with intracapsular femoral neck fractures treated with three cannulated screws placed in either a triangle or an inverted triangle configuration. J Bone Joint Surg Am. 2013; 95(1):61–69.Article Pubmed
[6]Li J, Wang M, Zhou J, Han L, Zang H, et al. Optimum configuration of cannulated compression screws for the fixation of unstable femoral neck fractures: finite element analysis evaluation. Biomed Res Int. 2018; 2018:1271762.Article Pubmed
[7]Garden RS. Malreduction and avascular necrosis in subcapital fractures of the femur. J Bone Joint Surg Br. 1971; 53(2):183–197.Article Pubmed
[8]EUR-Lex. Access to European Union law. Accessed from:https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX:32017R0745
[9]Kallan K, Åberg H, Berggren A, Ullman M, Snellman G, et al. Similar outcome of femoral neck fractures treated with Pinloc or Hansson Pins: 1-year data from a multicenter randomized clinical study on 439 patients. Acta Orthop. 2019; 90(6):542–546.Article Pubmed
[10]Berkes MB, Little MT, Lazaro LE, Cymerman RM, Helfet DL, et al. Catastrophic failure after open reduction internal fixation of femoral neck fractures with a novel locking plate implant. J Orthop Trauma. 2012; 26(10):170–176.Article Pubmed
[11]Fixation using alternative implants for the treatment of hip fractures (FAITH) investigators. Fracture fixation in the operative management of hip fractures (FAITH): an international, multicenter, randomized controlled trial. Lancet 2017; 389(10078):1519–1527.Article Pubmed



