Journal of Hepatology and Gastroenterology
An International Peer-Reviewed Open Access Journal
ISSN 2399-8199


- Download PDF
- |
- Download Citation
- |
- Email a Colleague
- |
- Share:
-
- Tweet
-

Journal of Hepatology and Gastroenterology
Volume 2, Issue 2, March 2017, Pages 7–11
Case reportOpen Access
Combined treatment of refractory ascites by alfapumpTM and surgical umbilical hernia repair in cirrhotic patients: Is this the right paradigm?
-
Nguyen Khac Eric1,*
 ,
Dharhi Abdennaceur2,
Petit Abir3,
Vaysse Benoit4,
Badaoui Rachid5,
Ormancey Fabrice6,
Lewandowski Elisabeth4 and
Regimbeau Jean-Marc2
,
Dharhi Abdennaceur2,
Petit Abir3,
Vaysse Benoit4,
Badaoui Rachid5,
Ormancey Fabrice6,
Lewandowski Elisabeth4 and
Regimbeau Jean-Marc2
- 1 Hepatology-Gastroenterology Unit, Amiens Picardie University Hospital Center, 80054 Amiens CEDEX 1, France
- 2 Digestive Surgery Unit, Amiens Picardie University Hospital Center, 80054 Amiens CEDEX 1, France
- 3 Central Pharmacy, Amiens Picardie University Hospital Center, 80054 Amiens CEDEX 1, France
- 4 Medical Information Department, Amiens Picardie University Hospital Center, 80054 Amiens CEDEX 1, France
- 5 Anesthesia-Resuscitation Department, Amiens Picardie University Hospital Center, 80054 Amiens CEDEX 1, France
- 6 Financial Department, Amiens University Hospital, Amiens Picardie University Hospital Center, 80054 Amiens CEDEX 1, France
*Corresponding author: Prof. Eric NGUYEN-KHAC, MD., PhD., Hepatology-Gastroenterology Unit, Amiens University Hospital, 80054 Amiens CEDEX 1, France. Tel.: 00 33 3 22 08 88 51; Fax: 00 33 3 22 08 96 83; E-mail: Nguyen-khac.eric@chu-amiens.fr
Received 29 November 2016 Revised 09 February 2017 Accepted 18 February 2017 Published 27 February 2017
DOI: http://dx.doi.org/10.14312/2399-8199.2017-2
Copyright: © 2016 Eric NK, et al. Published by NobleResearch Publishers. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
AbstractTop
Treatment of umbilical hernia in patients with refractory ascites due to cirrhosis is associated with a high risk of postoperative complications. Control of ascites must accompany and follow surgery in order to ensure adequate postoperative healing. The alfapump system is an innovative, rechargeable, fully implantable, automatic low-flow pump placed subcutaneously in the abdominal wall which automatically moves ascites from the peritoneal cavity to the bladder, thus decreasing or eliminating the need for paracentesis. We report the cases of two cirrhotic patients with both refractory ascites and large umbilical hernia who underwent repair of the umbilical hernia at the same time as alfapump system implantation. Implantation of the alfapump system resulted in control of ascites, improvement of nutritional status and quality of life, and no recurrence of the hernia. Combining implantation of the alfapump system with surgical repair of the umbilical hernia is offered as a possible solution to this therapeutic challenge.
Keywords: alfapump; automated low flow pump; refractory ascites; cirrhotic; transjugular intrahepatic portosystemic shunt (TIPS)
Study highlightTop
What is current knowledge? Treatment of umbilical hernia in cirrhosis patient with refractory ascite is a challenge.
What is new here? Combined treatment of refractory ascite by alfapump system and surgical umbilical hernia repair in the same operative time could be advantageous, with shortened hospital stay, no peritoneal drain, and less hernia recurrence.
IntroductionTop
Therapeutic management of umbilical hernias in patients with refractory ascites is a challenge [1-4]. We report, for the first time, a combination therapy for refractory cirrhotic ascites using a rechargeable automatic low-flow pump (the alfapumpTM system, Sequana Medical AG, Zurich, Switzerland), combined with concomitant surgical treatment for a dangerous umbilical hernia.
Case reportsTop
Patient 1
A 54-year-old man (BMI 24.2) had alcoholic cirrhosis Child-Pugh B7 since 2006. Large esophageal varices developed in 2008, treated with propanolol. In 2009, moderate ascites was treated with diuretics, complicated by spontaneous bacterial peritonitis. In 2013, he had bowel obstruction, related to strangulation of an umbilical hernia with massive ascites. The patient was hospitalized in the intensive care unit for treatment of renal failure with vasoactive amines and fluid replacement; subsequent surgical repair of the hernia by omphalectomy and placement of a peritoneal drain was performed. That drain was removed on day 13 and the patient was discharged on day 19. From 2013 to 2015, the ascites became refractory to high doses of diuretics (furosemide 80 mg a day, spironolactone 150 mg a day), required repeat paracentesis of 7 liters every 10 days, resulting in several acute kidney injury, and finaly a recurrence of the umbilical hernia. A transjugular intrahepatic portosystemic shunt (TIPS) had been considered, but was contraindicated, due to pulmonary arterial hypertension. On June 2015, a decision was made to combine implantation of a rechargeable alfapump in the abdominal wall to automatically transport the refractory ascites to the bladder. Surgical repair of the umbilical hernia was performed by placement of an intraperitoneal mesh without a peritoneal drain, during the same operation (Figure 1). Diuretics were discontinued. The alfapump was immediately activated, and the patient was out of bed on day 2, and after education on self-management of the alfapump, he was discharged on day 5. The alfapump daily target flow was gradually increased.
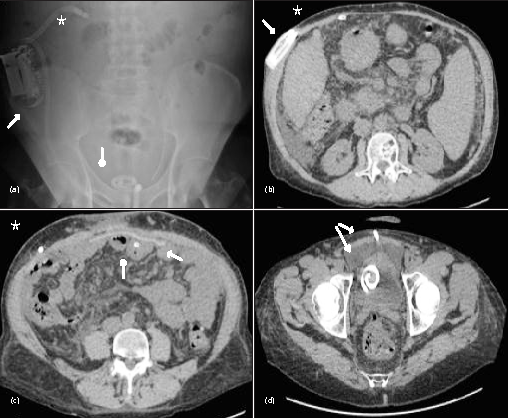
After 20 months follow up, the pump transported 520 liters of ascites (average of 0.951 liter per day) (Table 1, Figure 2). Hepatic function improved with a decrease in the MELD score, partly due to better renal function. With respect to quality of life, the patient had resumed physical activity the week after discharge with a daily 12-kilometer walk. The EQ-5D utility index and health state scores improved. The muscle circumferences of the triceps and quadriceps gradually increased. There was no acute kidney injury, infectious episodes, pump dislocation, poor urinary tolerance, and no recurrence of hernia. There were six periods of alfapump malfunction, at days 109 to 120, days 145 to 154, days 205 to 213, days 227 to 243, days 259 to 276, and days 370 to 380 relating to obstruction of the peritoneal catheter by the omentum, represented 12.9% of the total time. The first, third and fourth episodes was self-limiting. During the second episode, the catheter and pump were exchanged on day 154, due to obstruction by the omentum. During fifth episode, the peritoneal catheter was exchanged, due to omentum obstruction. Again, pump was exchanged during the sixth episode due to obstruction by omemtum (Figure 1). Three paracentesis were performed during follow up, at second, fifth and sixth periods of malfunction. At the time of the writing of this case report, the patient was doing well after 20 months.
| Patient 1 | ||||||||||||||||||
| alfapump (Liter) | INR | Bilirubin (µmol/L) | Albumin (g/L) | Creatinine (µmol/L) | MELD score | AST (IU/L) | ɣGT (IU/L) | Alk.P (IU/L) | Weight (kg) | Blood pressure Systol/diastol | Heart frequency/minute | Muscle Quadriceps (cm) | Muscle Triceps (cm) | Quality of Life EQ-5D | ||||
| Target volume per day | Total ascites transported | Ascites transported per day | Utility index score | Health state score | ||||||||||||||
| D0 | 0.346 | 0.325 | 0.325 | 1.4 | 14 | 31.2 | 123 | 13.3 | 43 | 365 | 130 | 70.0 | 112/52 | 60 | 39.5 | 21.2 | 0.365 | 50 |
| Week 2 | 0.75 | 10.02 | 0.680 ± 0.154 | 1.4 | 12.3 | 21 | 155 | 15.5 | 25 | 269 | 156 | 65.0 | 110/52 | 65 | 38.6 | 21.2 | 1.000 | 65 |
| Month 1 | 0.8 | 23.9 | 0.823 ± 0.187 | 1.2 | 8.1 | 31 | 124 | 11.5 | 40 | 429 | 296 | 63.5 | 100/50 | 81 | 38.7 | 21.2 | 1.000 | 70 |
| Month 2 | 1 | 53.7 | 0.942 ± 0.181 | 1.1 | 6.1 | 26 | 105 | 9.1 | 37 | 397 | 225 | 62.2 | 80/50 | 60 | 39.5 | 22.5 | 1.000 | 75 |
| Month 3 | 1 | 82.7 | 0.973 ± 0.156 | 1.1 | 5.8 | 27 | 96 | 8.2 | 45 | 416 | 221 | 68.5 | 90/50 | 53 | 42.3 | 23.6 | 1.000 | 75 |
| Month 4 | 1.1 | 109.9 | 0.972 ± 0.216 | 1.2 | 7.6 | 27 | 80 | 8.5 | 39 | 393 | 175 | 76.1 | 90/50 | 53 | 43.0 | 24.0 | 1.000 | 75 |
| Month 5 | 1.1 | 140.8 | 0.999 ± 0.259 | 1.2 | 4.7 | 26 | 110 | 10.5 | 36 | 378 | 216 | 78.9 | 100/50 | 54 | 45.0 | 24.0 | 0.888 | 70 |
| Month 6 | 1.2 | 162.8 | 0.958 ± 0.341 | 1.2 | 5.5 | 24 | 81 | 8.5 | 137 | 362 | 188 | 72.5 | 100/50 | 54 | 46.0 | 24.2 | 1.000 | 73 |
| Month 8 | 1.8 | 228.2 | 1.009 ± 0.410 | 1.1 | 5.9 | 28 | 92 | 7.8 | 32 | 369 | 219 | 79.1 | 110/60 | 61 | 46.0 | 25.4 | 0.888 | 71 |
| Month 9 | 1.4 | 248.4 | 0.977 ± 0.474 | 1.2 | 5.6 | 26 | 89 | 8.4 | 27 | 298 | 188 | 85.0 | 100/40 | 60 | 49.0 | 26.2 | 0.888 | 60 |
| Month 10 | 1.4 | 265.5 | 0.941 ± 0.502 | 1.1 | 6.3 | 24 | 74 | 7.5 | 29 | 270 | 190 | - | - | - | - | - | - | - |
| Month 13 | 1.1 | 362.1 | 0.989 ± 0.459 | 1.1 | 5.6 | 27 | 90 | 7.6 | 31 | 304 | - | 80.5 | 100/50 | 57 | 49 | 28.6 | 1.000 | 70 |
| Month 15 | 1 | 400.6 | 0.974 ± 0.441 | 1.2 | 6.8 | 25 | 79 | 8.4 | 27 | 262 | 159 | - | - | - | - | - | 1.000 | 70 |
| Month 17 | 1 | 446.6 | 0.960 ± 0.417 | 1.2 | 8.7 | 25 | 79 | 8.7 | 29 | 301 | 155 | - | - | - | - | - | 0.888 | 70 |
| Month 19 | 1 | 495.2 | 0.954 ± 0.396 | 1.2 | 8.5 | 27 | 81 | 8.4 | 26 | 296 | 141 | - | - | - | - | - | 1.000 | 75 |
| Month 20 | 1 | 519.7 | 0.951 ± 0.386 | 1.3 | 8 | 32 | 78 | 9.3 | 34 | 304 | 179 | 85.0 | 110/60 | 60 | 50.5 | 29.0 | 1.000 | 75 |
| Patient 2 | ||||||||||||||||||
| D0 | 0.166 | 0.426 | 0.426 | 1.73 | 20 | 32.1 | 94 | 13.7 | 32 | 75 | 108 | 76.7 | 100/50 | 54 | 42.0 | 25.2 | 0.487 | 65 |
| Week 2 | 0.8 | 5.392 | 0.674 ± 0.169 | 1.61 | 12 | 34.9 | 80.5 | 11.8 | 27 | 65 | 100 | 79.7 | 100/54 | 63 | 43.0 | 25.5 | 1.000 | 90 |
| Month 1 | 0.8 | 17.454 | 0.601 ± 0.395 | 1.76 | 13.4 | 25.3 | 69 | 12.7 | 22 | 69 | 93 | 85.2 | 120/60 | 66 | 42.0 | 25.4 | 0.844 | 95 |
| Month 2 | 0.8 | 51.461 | 0.903 ± 0.499 | 1.54 | 11.9 | 25.1 | 89.4 | 11.3 | 25 | 81 | 99 | - | - | - | - | - | - | 97 |
| Month 3 | 0.8 | 85.205 | 1.025 ± 0.438 | 1.66 | 10.2 | 25.3 | 79.7 | 12.1 | 24 | 89 | 99 | 80.0 | 100/50 | 61 | 42.0 | 26.2 | 1.000 | 98 |
| Month 4 | 1.2 | 115.482 | 1.021 ± 0.354 | 1.6 | 10 | 25.2 | 80.5 | 11.7 | 26 | 85 | 98 | - | - | - | - | - | - | 98 |
| Month 5 | 1.2 | 148.631 | 1.054 ± 0.354 | 1.56 | 8.5 | 26.4 | 77.9 | 11.4 | 26 | 86 | 99 | - | - | - | - | - | - | 98 |
| Month 6 | 1.2 | 178.806 | 1.058 ± 0.328 | 1.59 | 13.7 | 28.7 | 85.8 | 11.6 | 29 | 88 | 97 | 87.5 | 100/50 | 69 | 45.0 | 27.5 | 1.000 | 98 |
| Month 7 | 1.2 | 208.13 | 1.056 ± 0.311 | 1.69 | 15.4 | 28.8 | 80.5 | 12.3 | 28 | 79 | 104 | 88.0 | 100/60 | 70 | 45.0 | 28.0 | 1.000 | 98 |
| Month 8 | 1.2 | 234.32 | 1.041 ± 0.285 | 1.61 | 12 | 30.5 | 84.1 | 11.7 | 25 | 75 | 95 | 90.0 | 110/50 | 100 | 46.6 | 29.7 | 1.000 | 98 |
| Month 11 | 1.2 | 301.91 | 0.979 ± 0.281 | 1.52 | 13.7 | 31.7 | 85.8 | 11.1 | 26 | 77 | 96 | 92.0 | 110/60 | 70 | 47.0 | 29.8 | 1.000 | 98 |
| Month 12 | 1.2 | 322.79 | 0.959 ± 0.281 | 1.59 | 13.7 | 30 | 78.8 | 11.6 | 25 | 76 | 93 | 96.0 | 110/60 | 70 | 48.8 | 31.0 | 1.000 | 98 |
| Month 13 | 0.8 | 340.676 | 0.934 ± 0.282 | 1.56 | 11.9 | 30.4 | 78.8 | 11.4 | 28 | 77 | 98 | - | - | - | - | - | 1.000 | 98 |
| Month 14 | 0.8 | 356.57 | 0.908 ± 0.289 | 1.61 | 11.9 | 30.2 | 89.2 | 11.7 | 28 | 76 | 101 | 97.4 | 110/60 | 65 | 50.0 | 31.5 | 1.000 | 98 |
| Month 16 | 0.6 | 385.45 | 0.859 ± 0.301 | 2.26 | 13.6 | 33.6 | 81.4 | 15.5 | 25 | 70 | 84 | 98.0 | 140/70 | 72 | 51.5 | 32.5 | 1.000 | 98 |
| Month 20 | 0.6 | 434.8 | 0.775 ± 0.319 | 1.31 | 19 | 32 | 78 | 9.8 | 25 | 78 | 82 | 98.0 | 140/72 | 70 | 52.0 | 33.0 | 1.000 | 98 |
Note: 5Q-ED 3L: stated by patient for each item; Mobility, Self-Care, Usual activities, Pain/Disconfort, Anxiety/Depression (14). Health state score: Best imaginable health, stated by patient on a scale between “0” or worst health status and “100” or best health status.

Patient 2
A 62-year-old man (BMI 27.4) had Child-Pugh B (8) alcoholic cirrhosis, since 2008. There were no esophageal varices. He had moderate ascites, treated with diuretics and salt-free diet. In 2013, the ascites became refractory requiring repeat paracentesis of 9 liters every three weeks. The diuretics were lowered due to hypotension. The patient developed a painful umbilical hernia measuring 4 cm with skin ulceration. In the same operation, an alfapump was implanted and the umbilical hernia was repaired with omphalectomy and placement of a bioprosthesis, without peritoneal drain. The patient was out of bed on day 2. Diuretics were discontinued. The patient received education for self-management of the pump and then left the hospital on day 5. The alfapump daily target flow was gradually increase.
In 20 months follow up, the pump transported 435 liters of ascites (average of 0.775 liters per day) (Table 1, Figure 3). No paracentesis and no infusion of albumin were performed, and no ascites was detectable on ultrasound. The MELD score and renal function were stable, without infectious episodes, pump dislocation, poor urinary tolerance, or recurrence of hernia. Regarding quality of life, the utility index and health state scores improved. The muscle circumferences gradually increased. Pump malfunction occured between day 21 to day 34 (2.3% of the total time), possibly related to obstruction by the omentum. This only one single episode was self-limiting. This patient hadn’t need pump or catheter exchange during all follow up. At the time of the writing of this case report, the patient was doing well after 20 months.


DiscussionTop
In cirrhotic patients with refractory ascites and abdominal hernia symptoms such as pain, skin ulceration, or episodes of hernia strangulation, surgical repair is a challenge. The standardized mortality rate after surgery for an umbilical hernia is higher in patients with cirrhosis than without (3.9% versus 1%) [5], with higher morbidity and more need of intensive care unit [6]. Furthermore, emergency surgery is also a risk factor with a seven times higher mortality rate in patients with cirrhosis (3.8% vs. 0.5%) [6]. Control of ascites, before and after surgical repair of the hernia, is essential to prevent wound dehiscence due to ascites. A peritoneal drain is often left in place for a few days for that purpose. Surgical portosystemic shunt or a peritoneal-jugular shunt (LeVeen valve) [7] were proposed to control ascites, but these techniques are currently no longer in use [1]. For the same purpose, TIPS is recommended before or after hernia surgery [8], but requiring two general anesthesias, and is contraindicated in some patients with hepatic encephalopathy or with high MELD score.
Pilot series [9-11][9-11] and a randomized controlled trial [12] have shown a significant reduction in the need for paracentesis in patients with refractory ascites who underwent implantation of the alfapump system compared with the patients who were treated with conventional paracentesis [12]. The combination treatment strategy for refractory cirrhotic ascites by the alfapump system and surgical hernia repair has the theoretical advantages of reducing the hospitalization time, performing scheduled surgery with a lower theoretical mortality rate [6], avoiding placement of a peritoneal drain, and having only one anesthesia.
In our cases, there were no operative complications, and no need for a postoperative peritoneal drain, as the pump immediately treated the ascites, avoiding high abdominal pressure, risk of ascites leaking from the wound or resulting in skin dehiscence. Patient 1 underwent surgery initially for a strangulated umbilical hernia with refractory ascites two years ago. Postoperatively, there was renal failure, hemodynamic complications that required the use of vasoactive amines in the intensive care unit, placement of a peritoneal drain for nearly two weeks, and 19 days of hospitalization. The hernia ultimately recurred later, due to persistent refractory ascites. During the second operation for the recurrent hernia, there were no postoperative medical complications and no drain; hospitalization was only for 5 days.
At 20 months follow up, 520 liters of ascite (average of 0.951 liter per day) were transported in patient 1, and 435 liters of ascite (average of 0.775 liter per day) in patient 2. The amount of ascite transported by the alfapump were estimated at 6.6 liters a week for patient 1, and 5.4 liter a week for patient 2. We noted improved quality of life in both of our patients, with an improvement in muscle mass, no impairment of liver function, no kidney failure, brief need for paracentesis only in patient 1, definitive stop of diuretics, and no recurrence of hernia. Interestingly, no albumin infusion were required. We believe that oral nutrition was easier when ascite is controlled by a continue transport by the pump, and than nutritional status improved, Recent study report a better quality of life in patient implanted with alfapump [13].
Alfapump malfunction occurred in 12.9% and 2.3% of the total time 20 months follow up, respectively in patients 1 and 2. Malfunction could be self limiting, due to omentum aspiration by the peritoneal catheter. However, when the omemtum is aspirated by the catheter and reaches the pump, the pump is set to crush it. Despite this algorithm, the pump was changed two times for a complete blockage in patient 1. In a less damaging way, omemtum can block only the peritoneal catheter requiring his replacement. A new designed peritoneal catheter was implantated at last exchange in patient 1, avoiding all pump malfunction after. For patient 2, no catheter or pump exchanges were necessary.
ConclusionTop
This combination therapy simultaneously treats refractory ascites and allows for surgical repair of the umbilical hernia in difficult cirrhotic patients. The efficacy of this treatment combination should be confirmed by a larger series of patients.
Conflicts of interest
The authors declare no conflicts of interest.
ReferencesTop
[1]European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010; 53(3):397–417.Article Pubmed
[2]Sabbagh C, Fuks D, Regimbeau JM. Non-hepatic gastrointestinal surgery in patients with cirrhosis. J Visc Surg. 2014; 151(3):203–211.Article Pubmed
[3]Dokmak S, Aussilhou B, Belghiti J. Umbilical hernias, cirrhosis. J Visc Surg. 2012; 149(5 Suppl):e32–39.Article Pubmed
[4]Belghiti J, Durand F. Abdominal wall hernias in the setting of cirrhosis. Semin Liver Dis. 1997; 17(3):219–226.Article Pubmed
[5]Hansen JB, Thulstrup AM, Vilstup H, Sørensen HT. Danish nationwide cohort study of postoperative death in patients with liver cirrhosis undergoing hernia repair. Br J Surg. 2002; 89(6):805–806.Article Pubmed
[6]Carbonell Alfredo M, Wolfe Luke G, DeMaria Eric J. Poor outcomes in cirrhosis-associated hernia repair: A nationwide cohort study of 32,033 patients. Hernia. 2005; 9(4):353–357.Article Pubmed
[7]Belghiti J, Desgrandchamps F, Farges O, Fékété F. Herniorrhaphy and concomitant peritoneovenous shunting in cirrhotic patients with umbilical hernia. World J Surg. 1990; 14(2): 242–246.Article Pubmed
[8]Fagan SP, Awad SS, Berger DH. Management of complicated umbilical hernias in patients with end-stage liver disease and refractory ascites. Surgery. 2004; 135(6):679–682.Article Pubmed
[9]Bellot P, Welker MW, Soriano G, von Schaewen M, Appenrodt B, et al. Automated low flow pump system for the treatment of refractory ascites: a multi-center safety and efficacy study. J Hepatol. 2013; 58(5):922–927.Article Pubmed
[10]Stirnimann G, Berg T, Spahr L, Zeuzem S, McPherson S, et al. Alfapump for the treatment of refractory ascites in cirrhotic patients. J Hepatol. 2015; 62(Suppl 2):P0136–S352.Article
[11]Adebayo D, Mohammed A, Arora S, De Chiara F, Trepte C, et al. A Randomized controlled trial comparing the alfapump© with paracentesis in patients with refractory ascites: Clinical and pathophysiological effects on cardiac, haemodynamic, inflammatory, renal and nutritional parameters. J Hepatol. 2015; 62 (Supple 2):P0137–S374.Article
[12]Adebayo D, Bureau C, de Rieu MC, Valla D, Elkrief L, et al. Alfapump® system versus large volume paracentesis in the treatment of refractory ascites; results from a multicenter randomised controlled study (RCT). J Hepatol. 2016; 64(2):S185.Article
[13]Younossi ZM, Stepanova M, Nader F, Hunt S, Bureau C, et al. Patients with Refractory Ascites Treated with alfapump® System (AP) have Better Health-related Quality of Life (HRQL) as Compared to those Treated with Large Volume Paracentesis (LVP): Results of a Multicenter Randomized Controlled Study (Poster Abstract). Hepatology. 2016; 64(Supple 1):2077.


