Journal of Clinical and Interventional Cardiology
An International Peer-Reviewed Open Access Journal
ISSN 2399-8202

- Download PDF
- |
- Download Citation
- |
- Email a Colleague
- |
- Share:
-
- Tweet
-

Journal of Clinical and Interventional Cardiology
Volume 5, Issue 1, January 2023, Pages 1–6
Original researchOpen Access
Length of stay and 30 day mortality in patients suffering an uncomplicated ST-elevation myocardial infarction treated with primary percutaneous coronary intervention in New York State
-
Neil D. Shah1,*, MD,
 , Gregory W. Yost1, DO, Edward L. Hannan2, PhD, Ye Zhong2, MD, Ferdinand J. Venditti3, MD, David R. Holmes4, Jr., MD, Nicholas Stamato5, MD, Samin K. Sharma6, MD, Alice K. Jacobs7, MD, Spencer B. King Iii8MD and
Peter B. Berger9, MD
, Gregory W. Yost1, DO, Edward L. Hannan2, PhD, Ye Zhong2, MD, Ferdinand J. Venditti3, MD, David R. Holmes4, Jr., MD, Nicholas Stamato5, MD, Samin K. Sharma6, MD, Alice K. Jacobs7, MD, Spencer B. King Iii8MD and
Peter B. Berger9, MD
- 1 Department of Cardiology, Geisinger Medical Center, Danville, PA, USA
- 2 School of Public Health, University at Albany, Albany, NY, USA
- 3 Department of Clinical Affairs, Albany Medical College, Albany, NY, USA
- 4 Department of Cardiology, Mayo Clinic, Rochester, MN, USA
- 5 Department of Cardiology, United Health Services Hospitals, Johnson City, NY, USA
- 6 Department of Cardiology, Mount Sinai Medical Center, New York, NY, USA
- 7 Department of Cardiology, Boston Medical Center, Boston, MA, USA
- 8 Division of Cardiology, Department of Medicine, Emory Healthcare, Atlanta, GA, USA
- 9 Northwell Health Professor of Cardiology and Medicine-Hofstra, Northwell School of Medicine, Great Neck, NY, USA
*Corresponding author: Neil D. Shah, MD., Geisinger Medical Center, 100 N Academy Ave, Danville, PA 17821, USA. Tel.: 570-271-6523; Email: nshah3@geisinger.edu
Received 13 October 2022 Revised 17 December 2022 Accepted 26 December 2022 Published 3 January 2023
DOI: http://dx.doi.org/10.14312/2399-8202.2023-1
Copyright: © 2022 Shah ND, et al. Published by NobleResearch Publishers. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
AbstractTop
We studied the duration of hospitalization and clinical outcome of patients with an uncomplicated STEMI (ST-elevation myocardial infarction) treated with primary percutaneous coronary intervention (PCI) in New York State between 2007 and 2009. Among the 4,939 such patients, 1,818 were discharged after 2 nights, and 1,922 were discharged after 3 nights. There were no deaths on the day after discharge among patients discharged after 2 nights. There was also no significant difference in 30-day mortality or readmission between patients discharged after 2 and 3 nights. In conclusion, 24-hour mortality was very low in patients with an uncomplicated STEMI discharged after 2 nights in the hospital, based on physician judgment. Thirty-day mortality is also low and similar to that of patients discharged after 3 nights in the hospital.
Keywords: STEMI; length of stay; discharge; readmission; myocardial infarction; coronary intervention
IntroductionTop
Early and complete restoration of coronary blood flow reduces morbidity and mortality from acute ST-elevation myocardial infarction (STEMI) [1-4]. It may also lead to a reduction in the length of hospital stay. Decreasing hospital length of stay should substantially reduce cost, an important consideration in this era of financial constraints [5]. In recent years, several small studies have investigated the appropriate timing of discharge following a STEMI for which primary percutaneous coronary intervention (PCI) is performed [6-10]. The European Society of Cardiology (ESC) guidelines state that in low-risk patients successfully treated with primary PCI after uncomplicated myocardial infarction (MI), it is safe and feasible to consider early discharge (within 72 hours) [11]. No such recommendations exist in the current ACC/AHA STEMI guidelines about when patients may be safely discharged [12]. Despite several studies aiming to identify appropriate lengths of stay following an uncomplicated MI there exists much variability. Many variables factor into timing of patient discharge but in certain low-risk situations discharging a patient a day earlier (2 nights Vs. 3 nights) may be safer (e.g., reduce risk of nosocomial infection) and more cost-effective.
We hypothesized that many patients suffering an uncomplicated STEMI who undergo a PCI procedure can be safely discharged after 2 nights in the hospital. To test this hypothesis, we performed this retrospective cohort analysis of the New York State PCI registry to determine the length of stay (2 nights Vs. 3 nights) after an uncomplicated STEMI treated with PCI, and the relationship between day of discharge and survival at 24 hours and 30 days.
MethodsTop
The primary database used in this study was the New York State (NYS) Percutaneous Coronary Interventions Reporting System (PCIRS) registry, which was developed in 1991 for the purpose of collecting information on all patients undergoing PCI in New York’s non-Federal hospitals. PCIRS contains detailed information for each patient undergoing PCI in the state regarding demographics; pre-procedural risk factors; peri-procedural complications; types of devices used; extent of disease and lesions treated; dates of admission, discharge and procedure; discharge disposition and destination; and hospital and operator identifiers. The data are collected by hospital catheterization laboratories, entered on paper forms and then submitted to the New York State Department of Health (NYSDOH) on diskettes or through a web-based submission process. The data are checked for accuracy and completeness by matching to administrative data and by extensive auditing of medical records by the NYSDOH’s utilization review agent. We used the Social Security Death Index and New York’s Vital Statistics data to identify deaths that occurred after discharge [13]. Data on readmission are obtained from the Department of Health’s acute care hospital dataset, the Statewide Planning and Research Cooperative System (SPARCS), which contains data pertaining to all acute care hospital discharges in the state. Thirty-day readmission is defined as admission to a NYS non-Federal hospital within 30 days of discharge from the index hospitalization when the second admission is not for the purpose of staged PCI.
We examined the NYS PCI Registry and identified all patients who suffered a STEMI and underwent primary PCI (PCI within 12 hours of symptom onset; n=13,399) between 2007 and 2009. Information about individual patients was de-identified prior to data compilation and analysis. We excluded patients for whom the PCI procedure was unsuccessful or who suffered a complication of the PCI procedure. We also excluded patients with symptomatic congestive heart failure or malignant ventricular arrhythmias prior to the STEMI incident and patients with complications from their STEMI, including cardiogenic shock or hemodynamic instability. Patients with a left ventricular ejection fraction (LVEF) <40% were also excluded, as were patients with creatinine >2.0mg/dL or requiring dialysis. Patients with LVEF <40% were excluded because they are at markedly higher risk for the development of arrhythmia and heart failure. We excluded patients who lived outside the USA for whom vital status at 30 days might not be obtainable, patients who were transferred to another hospital during the index hospitalization, those who left the hospital against medical advice or on the first hospital day for any reason, and patients who remained in the hospital for more than 3 nights (Table 1). Patients with hospitalizations for 4 nights or longer were not analyzed because many such patients may have had other cardiac or non-cardiac illnesses (or discharge disposition issues) that may have provided an explanation for longer hospitalization that could not be identified in this database. In this study, we sought to narrowly examine the frequency of discharge after 2 Vs. 3 nights after an uncomplicated, low-risk STEMI treated with PCI, and compare the safety of those 2 practices. The length of stay for patients was counted as number of nights stayed in the hospital rather than number of days, or hours, in part because that is how payers determine length of stay.
N (%) |
# of patients left |
||
| Number of STEMI (MI <12 hours) patients in 2007-2009 | 13,399 |
-- |
|
| Exclusions | |||
| Received thrombolytic before PCI | 440 (3.28%) |
12,318 |
|
| Died in hospital | 286 (2.13%) |
11,878 |
|
| Complication of the PCI* | 319 (2.38% ) |
11,559 |
|
| Shock | 137 (1.02%) |
11,422 |
|
| Hemodynamically unstable | 297 (2.21%) |
11,125 |
|
| Severe comorbidity Creatinine >2.0 or renal failure requiring dialysis Malignant ventricular arrhythmia Congestive heart failure |
>679 (5.07%) |
10,446 |
|
| Ejection fraction <40% | 4,540 (33.9%) |
5,906 |
|
| Transferred to another acute care facility | 96 (0.72%) |
5,810 |
|
| Out of country | 4 (0.03%) |
5,806 |
|
| Same day discharge | 9 (0.07%) |
5,797 |
|
| Discharged after >4 nights | 858 (6.4%) |
4,939 |
|
Abbreviations: STEMI: ST-segment elevation myocardial infarction, MI: Myocardial infarction, PCI: Percutaneous coronary intervention, * Complication includes major events following PCI: stroke, Q-Wave MI, acute occlusion in the targeted lesion, acute occlusion in a significant side branch, A/V injury at cath entry site (requiring intervention), renal failure, emergency cardiac surgery, stent thrombosis, emergency return to cath lab for PCI, and coronary perforation..
Patient risk factors (anatomic and procedural data, as well as demographics and clinical characteristics) were compared between patients who spent 2 Vs. 3 nights in the hospital using the Chi-square test for discrete variables and using the Wilcoxon Rank Sum test for comparing the medians of continuous variables. Readmission rates and the frequency and timing of deaths occurring within 30 days of discharge were also compared for patients discharged after 2 nights and 3 nights in the hospital. Results with p-value < 0.05 were considered significant.
ResultsTop
A total of 13,399 patients were diagnosed with acute STEMI and underwent PCI in New York between January 1, 2007 and December 31, 2009. After excluding patients not meeting the inclusion criteria (Table 1), 4,939 patients (36.9% of all STEMI patients) were considered to have had an uncomplicated STEMI and PCI. Their mean age was 58.2±12.1 years; most patients were male (75.1%) and white (83.3%). Most patients presented within 6 hours of symptom onset (84.7%), had no previous PCI procedures (87.7%), and had single or no vessel disease (59.7%) (Tables 2 and 3). Their median ejection fraction was 51%.
All patients n=4,939* |
Discharged after 2 nights (%) n=1,818 |
Discharged after 3 nights (%) n=1,922 |
P-value (After 2 nights vs. After 3 nights) |
||
| Left main disease | 1.5 |
1.3 |
1.9 |
0.14 |
|
| Number of vessels diseased | 0.003 |
||||
| One or none | 59.7 |
63.8 |
58.4 |
||
| Two | 30.1 |
27.9 |
31.3 |
||
| Three | 10.2 |
8.4 |
10.3 |
||
| Ejection fraction (%) | <0.0001 |
||||
| 40-49 | 28.6 |
23.7 |
31.3 |
||
| >=50 | 71.4 |
76.4 |
68.7 |
||
| Time from MI symptom onset | 0.44 |
||||
| < 6hr | 84.7 |
85.7 |
84.8 |
||
| ≥ 6 and < 12 hours | 15.3 |
14.3 |
15.2 |
||
Abbreviations: MI: Myocardial infarction.
All patients n=4,939* |
Discharged after 2 nights n=1,818 |
Discharged after 3 nights n=1,922 |
P-value (After 2 nights Vs. after 3 nights) |
||
| Median age (yr.) | 57 |
56 |
57 |
0.003 |
|
| Mean age (yr.) | 58.2±12.1 |
57.1±11.4 |
58.3±12.1 |
0.002 |
|
| Female gender (%) | 24.9 |
21.7 |
26.4 |
0.0009 |
|
| Hispanic ethnic (%) | 10.2 |
8.0 |
10.6 |
0.007 |
|
| Race (%) | 0.04 |
||||
| White | 83.3 |
85.0 |
82.3 |
||
| Black | 8.8 |
8.3 |
9.0 |
||
| Others | 7.9 |
6.7 |
8.7 |
||
| BMI (%) | 0.41 |
||||
| < 16.5 | 0.2 |
0.2 |
0.2 |
||
| 16.5-18.4 | 0.8 |
0.9 |
0.5 |
||
| 18.5-24.9 | 20.8 |
20.2 |
20.6 |
||
| 25.0-30.0 | 42.8 |
42.5 |
43.5 |
||
| 20.1-34.9 | 23.0 |
24.6 |
22.5 |
||
| 35.0-40.0 | 8.3 |
8.0 |
8.7 |
||
| > 40.0 | 4.1 |
3.6 |
4.1 |
||
| Previous PCI (%) | 12.3 |
12.7 |
11.5 |
0.26 |
|
| Carotid/ cerebrovascular disease (%) | 2.8 |
2.4 |
2.7 |
0.58 |
|
| Peripheral vascular disease (%) | 2.5 |
2.5 |
2.1 |
0.36 |
|
| Chronic obstructive pulmonary disease (%) | 3.0 |
2.3 |
3.2 |
0.09 |
|
| Diabetes (%) | 16.3 |
15.1 |
16.2 |
0.38 |
|
| Renal failure (%) | 0.09 |
||||
| Creatinine: < 1.2 mg/dl, no dialysis | 74.3 |
75.7 |
75.4 |
||
| Creatinine: 1.2-1.5 mg/dl, no dialysis | 21.9 |
21.8 |
21 |
||
| Creatinine: 1.6-2.0 mg/dl, no dialysis | 3.3 |
2.4 |
3.6 |
||
| Previous cardiac surgery (%) | 2.8 |
2.4 |
2.4 |
0.96 |
|
| Organ transplant (%) | 0.2 |
0.2 |
0.2 |
0.76 |
|
Abbreviations: BMI: Body mass index, PCI: Percutaneous coronary intervention..
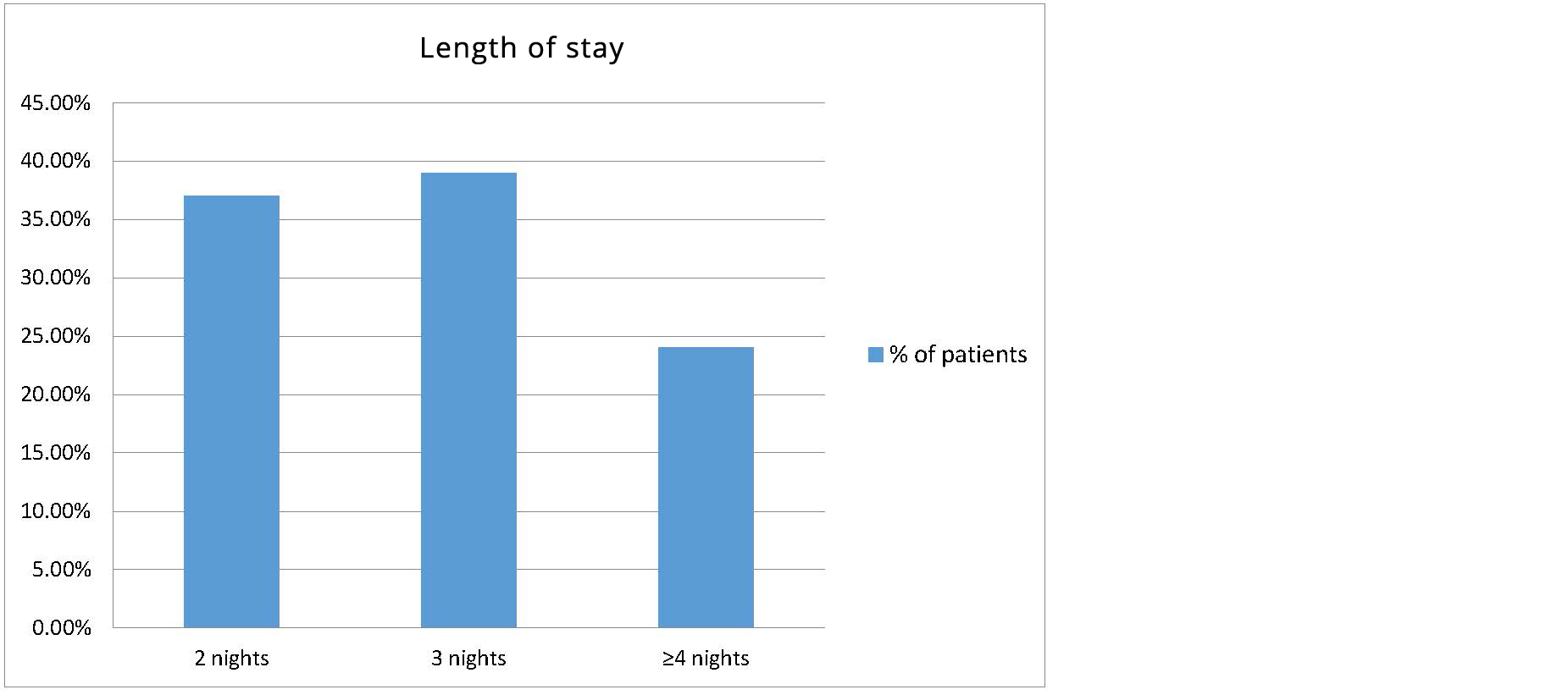
More than 1/3 of patients in the study population were discharged after 2 nights in the hospital (n=1,818; 36.8% of the uncomplicated STEMI patients in the study population), and 1,922 (38.9%) patients were discharged after 3 nights in the hospital. The 1,199 (24.2%) uncomplicated STEMI patients discharged after 4 or more nights in the hospital were not analyzed further (Figure 1).
The baseline clinical characteristics of the study population are displayed in Table 3. Patients who were discharged after only 2 nights of hospitalization were younger, more likely to be male, white, and non-Hispanic than patients with 3 night hospital stays.
Patients discharged after only 2 nights in the hospital had a greater mean left ventricular ejection fraction (LVEF) and were more likely to have single-vessel disease than patients discharged after 3 nights.
All-cause readmission rates were compared between the patients discharged after 2 nights and 3 nights. There were 458 patients (12.2%) readmitted within 30 days of the PCI. Of these, 136 patients (29.6%) were readmitted for a planned staged PCI. There was no difference in the frequency of readmission for reasons other than a planned PCI (n=156, 8.9% Vs. n=166, 9.0%; p=0.89) or for a staged PCI (n=59, 3.2% Vs. n=77, 4.0%; p=0.21) between patients discharged after 2 versus 3 nights (Table 4).
# of patients |
Staged PCI |
# of Patients without staged PCI |
30-day readmission |
|||
N (%) |
P-value |
N (%) |
P-value |
|||
| 2-night hospitalization | 1,818 |
59 (3.2%) |
0.21 |
1,759 |
156 (8.9%) |
0.89 |
| 3-night hospitalization | 1,922 |
77 (4.0%) |
1,845 |
166 (9.0%) |
||
| Total | 3,740 |
136 (3.6%) |
3,604 |
322 (8.9%) |
||
None of the 1,818 patients discharged after 2 nights died the following day. 2 of the 1,922 patients discharged after 3 nights died on the following day (0.1%).
There was no significant difference in 30-day mortality between patients discharged after 2 nights (n=4, 0.22%) Vs. after 3 nights (n=3, 0.16%).The earliest patient death in the 2 night discharge group occurred on the 6th day after discharge. The earliest death in the 3 night discharge group occurred on the 1st day after discharge (Tables 5 and 6).
N |
||
| Total number of patients discharged after 2 nights in hospital following PCI | 1,818 (36.8%*) |
|
| Total death in 30 days after PCI | 4 (0.22%) |
|
| Death time | ||
| 6th Day after discharge | 1 |
|
| 18 Day after discharge | 1 |
|
| 20 Day after discharge | 1 |
|
| 27 Day after discharge | 1 |
|
| Total | 4 |
|
Abbreviations: PCI: Percutaneous coronary intervention, *Percentage among 4,939 patients who were discharged in 1-4 days.
N |
||
| Total number of patients discharged after 3 nights in hospital following PCI | 1,922 (38.9%*) |
|
| Total death in 30 days after PCI | 3 (0.16%) |
|
| Death time | ||
| 1st Day after discharge | 2 |
|
| 17 Day after discharge | 1 |
|
| Total | 3 |
|
Abbreviations: PCI: Percutaneous coronary intervention, *Percentage among 4,939 patients who were discharged in 1-4 days.
DiscussionTop
The most important finding from this retrospective analysis of a large number of patients in New York State who underwent successful primary PCI for a STEMI is that about 40% of them had no pre-existing comorbidities (e.g., congestive heart failure, malignant ventricular arrhythmias, end-stage renal disease requiring dialysis) or complications from the time of onset of symptoms of the STEMI through the first 2 days in the hospital. In such patients, early discharge -- after 2 nights in the hospital, instead of 3 nights or longer -- appears to be safe. No significant difference between 30-day readmission rates was found. There were no deaths in the day following discharge, and the mortality rate at 30 days was very low and similar to that of patients who remained in the hospital for 3 nights.
Prior studies have shown potential feasibility and safety of discharging patients at 48 hours (or <72 hours) if they experienced an uncomplicated MI [6, 8-10]. Over the past few decades, there have been tremendous advances in therapy for acute coronary syndromes. Therapeutic improvements have decreased hospital lengths of stay for patients from weeks to days. Initially, when fibrinolytic therapy was routinely administered to STEMI patients, studies revealed that the extent and size of infarction was limited and thus ventricular function and mortality had improved. These beneficial results were noted to be even better the earlier the infarct-related artery was reperfused [5, 14-16]. Studies by Topol and Grines and Newby found that discharge after 3 or more days appeared to be safe in the reperfusion era, and that there is a substantial reduction in cost when patients were discharged earlier than had traditionally been the practice [5, 17, 18]. More recently, with the recognition that most patients suffering a STEMI ought to undergo primary PCI, studies have shown better patency rates, fewer major complications and advantages in outcomes for patients undergoing early angioplasty versus thrombolytic therapy [1-4, 17]. In multiple studies comparing early discharge (<72 hours or ≤ days) Vs. later in patients felt to be low risk following PCI after STEMI, the shorter lengths of stay have not been associated with increased mortality in the setting of an uncomplicated MI [6, 8, 19-22]. This observation is critically important to physicians when making discharge decisions.
Our study provides data that further helps to substantiate the safety of early discharge. Analyses of the ACC NCDR indicate that a quarter of STEMI patients treated with primary PCI are now discharged after 2 nights in the hospital, but until more recently data suggesting that this practice is safe had been scant [21, 2]. It is important to establish whether safe, early discharge results can be reproduced in different settings in the current era where primary PCI is the mainstay of treatment in acute STEMI as opposed to older studies when PCI was not the standard of care [18].
Prognostic scoring systems have been used to identify patients having an uncomplicated MI or considered low risk for future complications [6, 9, 23]. Similar to our study, other studies did not use a scoring system to delineate a group of patients who could be discharged early but were still able to prove there was no difference in mortality rate [8, 10]. While scoring systems may be a helpful guide, the ultimate decision on discharge depends on the clinician’s assessment of each individual patient. The reproduction of outcomes in multiple settings over time using therapies considered standard of care reinforces the idea that when a patient has been appropriately identified as low risk or having an uncomplicated MI, it is reasonable and safe to discharge the patient after 2 nights in the hospital.
The goal of this study was to highlight that a group of patients with uncomplicated, low-risk MIs could be safely discharged early. Uncomplicated MIs were defined as patients surviving primary percutaneous coronary intervention and suffered none of the following: stroke, Q-Wave MI, acute occlusion in the targeted lesion, acute occlusion in a significant side branch, A/V injury at cath entry site (requiring intervention), renal failure, emergency cardiac surgery, stent thrombosis, emergency return to cath lab for PCI, and coronary perforation (Table 1). We hoped to demonstrate the likelihood of having a complication or mortality in low-risk STEMI patients discharged after 2 nights following hospitalization for an uncomplicated MI is very low. After exclusions, 6,305 patients meeting definition of uncomplicated MI were treated with PCI. Comparison of patients discharged after 2 nights (n=1,818) Vs. after 3 nights (n=1,922) found the latter discharge group tended to be older, and more likely to be female, of Hispanic ethnicity, non-white, have lower ejection fractions and more diseased coronary vessels. Despite these disparities the mortality rates for both groups was extremely low and there was no significant difference in mortality between patients discharged after 2 nights Vs. 3 nights. Additionally, there was no difference in 30-day readmission between the 2 groups of patients. Despite our study including patients all of ages, these results are similar to those previously described by Swaminathan et al which included only patients ≥ years [22]. This supports our hypothesis - following a low-risk uncomplicated MI, discharging a patient after 2 nights instead of keeping an additional day is very unlikely to miss a significant negative or sentinel event that may ultimately lead to mortality.
Advances in technical and medical therapeutics have profoundly impacted the outcomes of patients after an acute STEMI. In addition to improving outcomes they have shortened the duration of hospital stay for a patient reducing the risk of other possible detrimental outcomes (i.e., acquiring nosocomial infection, psychological depression, and reduced mobilization). This can soften overall health care costs by reducing hospital stay without putting patients at higher risk for later complications. Arguments may be made that discharging patients too early following an acute MI may miss the opportunity for educating them regarding their disease, implementing lifestyle modifications, and prescribing and discussing secondary prevention medications. While this study may not address this question head on, it does support the notion that there were no near term adverse outcomes in the 2 night discharge group. Previous studies done in other countries have provided evidence to support discharge timing recommendations in the European STEMI guidelines. The results shown in this study are not intended to establish standard of care but rather support physicians who feel it is safe to discharge a patient after 2 nights following an uncomplicated STEMI. We hope these data offer support to physicians and future STEMI guidelines committee members that early discharge of many patients who suffer an uncomplicated, low-risk STEMI (after 2 nights in the hospital) appears to be safe.
While this retrospective cohort study has analyzed data submitted to the New York State Department of Health PCI registry for the years 2007-2009, data about the antithrombotic and other medical therapy that such patients received could not be obtained. We were unable to be more granular about the length of stay (i.e., specific timing of admission and discharge, measured in hours rather than nights in the hospital). There may have been reasons that patients suffering an uncomplicated STEMI were hospitalized for longer periods of time that were not captured in our analyses (e.g., medical problems unrelated to the STEMI, discharge disposition); therefore, our data ought to be applied only to patients with an uncomplicated STEMI (i.e., not meeting our suggested exclusion criteria) for whom the attending physician thought that early discharge was appropriate. Unmeasured variables may be able to characterize patients for whom longer periods of hospitalization may be appropriate.
ConclusionTop
Patients who had been successfully treated by PCI after an uncomplicated STEMI and were discharged after 2 nights, based on physician judgment, in the hospital had a very low frequency of adverse events in the following day, and both 30-day mortality and need for readmission were low, similar to that of patients discharged after 3 nights in the hospital. This study suggests that the potential exists for a significant reduction in the cost of care required for STEMI patients without harming outcomes at all.
Conflicts of interest
Authors declare no conflict of interest.
ReferencesTop
[1]Figueras J, Alcalde O, Barrabes JA, Serra V, Alguersuari J, et al. Changes in hospital mortality rates in 425 patients with acute ST-elevation myocardial infarction and cardiac rupture over a 30-year period. Circulation. 2008; 118(25):2783–2789.Article Pubmed
[2]The Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes (GUSTO IIb) Angioplasty Substudy Investigators. A clinical trial comparing primary coronary angioplasty with tissue plasminogen activator for acute myocardial infarction. N Engl J Med. 1997; 336(23):1621–1628.Article Pubmed
[3]Berger PB, Ellis SG, Holmes DR, Granger CB, Criger DA, et al. Relationship between delay in performing direct coronary angioplasty and early clinical outcome in patients with acute myocardial infarction: results from the global use of strategies to open occluded arteries in Acute Coronary Syndromes (GUSTO-IIb) trial. Circulation. 1999; 100(1):14–20.Article Pubmed
[4]Stone GW. Angioplasty strategies in ST-segment-elevation myocardial infarction: part I: primary percutaneous coronary intervention. Circulation. 2008; 118(5):538–551.Article Pubmed
[5]Topol EJ, Burek K, O'Neill WW, Kewman DG, Kander NH, et al. A randomized controlled trial of hospital discharge three days after myocardial infarction in the era of reperfusion. N Engl J Med. 1988; 318(17):1083–1088.Article Pubmed
[6]Kotowycz MA, Cosman TL, Tartaglia C, Afzal R, Syal RP, et al. Safety and feasibility of early hospital discharge in ST-segment elevation myocardial infarction--a prospective and randomized trial in low-risk primary percutaneous coronary intervention patients (the Safe-Depart Trial). Am Heart J. 2010; 159(1):117.e1–117.e6.Article Pubmed
[7]Laarman GJ, Dirksen MT. Early discharge after primary percutaneous coronary intervention. Heart. 2010; 96(8):584–587.Article Pubmed
[8]Karabulut A, Cakmak M, Uzunlar B, Bilici A. What is the optimal length of stay in hospital for ST elevation myocardial infarction treated with primary percutaneous coronary intervention? Cardiol J. 2011; 18(4):378–384.Article Pubmed
[9]Jones DA, Rathod KS, Howard JP, Gallagher S, Antoniou S, et al. Safety and feasibility of hospital discharge 2 days following primary percutaneous intervention for ST-segment elevation myocardial infarction. Heart. 2012; 98(23):1722–1727.Article Pubmed
[10]Noman A, Zaman AG, Schechter C, Balasubramaniam K, Das R. Early discharge after primary percutaneous coronary intervention for ST-elevation myocardial infarction. Eur Heart J Acute Cardiovasc Care. 2013; 2(3):262–269.Article Pubmed
[11]Task Force Members, Steg PG, James SK, Atar D, Badano LP, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Eur Heart J. 2012; 33(20):2569–2619.Article Pubmed
[12]O'Gara PT, Kushner FG, Ascheim DD, Casey DE, Chung MK, et al. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: Executive Summary: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: Developed in Collaboration With the American College of Emergency Physicians and Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv. 2013; 82(1):E1–E27.Article Pubmed
[13]Percutaneous coronary angioplasty in New York State: 2007–2009. Accessed June 21, 2014 from:https://www.health.ny.gov/statistics/diseases/cardiovascular/docs/pci_2007-2009.pdf
[14]ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Randomised trial of intravenous streptokinase, oral aspirin, both or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. Lancet. 1988; 2(8607):349–360.Article Pubmed
[15]GUSTO Angiographic Investigators. The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function, and survival after acute myocardial infarction. N Engl J Med. 1993; 329(22):1615–1622.Article Pubmed
[16]White HD, Van de Werf FJJ. Thrombolysis for Acute Myocardial Infarction. Circulation. 1998; 97(16):1632–1646.Article Pubmed
[17]Grines CL, Marsalese DL, Brodie B, Griffin J, Donohue B, et al. Safety and cost-effectiveness of early discharge after primary angioplasty in low risk patients with acute myocardial infarction. PAMI-II Investigators. Primary Angioplasty in Myocardial Infarction. J Am Coll Cardiol. 1998; 31(5):967–972.Article Pubmed
[18]Newby LK, Eisenstein EL, Califf RM, Thompson TD, Nelson CL, et al. Cost effectiveness of early discharge after uncomplicated acute myocardial infarction. N Engl J Med. 2000; 342(11):749–755.Article Pubmed
[19]Spencer FA, Lessard D, Gore JM, Yarzebski J, Goldberg RJ. Declining length of hospital stay for acute myocardial infarction and postdischarge outcomes: a community-wide perspective. Arch Intern Med. 2004; 164(7):733–740.Article Pubmed
[20]Berger AK, Duval S, Jacobs DR, Barber C, Vazquez G, et al. Relation of length of hospital stay in acute myocardial infarction to postdischarge mortality. Am J Cardiol. 2008; 101(4):428–434.Article Pubmed
[21]Chin CT, Weintraub WS, Dai D, Mehta RH, Rumsfeld JS, et al. Trends and predictors of length of stay after primary percutaneous coronary intervention: A report from the CathPCI Registry. Am Heart J. 2011; 162(6):1052–1061.Article Pubmed
[22]Swaminathan RV, Rao SV, McCoy LA, Kim LK, Minutello RM, et al. Hospital length of stay and clinical outcomes in older STEMI patients after primary PCI: a report from the National Cardiovascular Data Registry. J Am Coll Cardiol. 2015; 65(12):1161–1171.Article Pubmed
[23]Luca GD, Suryapranata H, van't Hof AWJ, Boer MJ, Hoorntje JCA, et al. Prognostic assessment of patients with acute myocardial infarction treated with primary angioplasty: implications for early discharge. Circulation. 2004; 109(22):2737–2743.Article Pubmed


